Beyond renal dialysis and transplantation – implantable artificial kidneys
Abstract
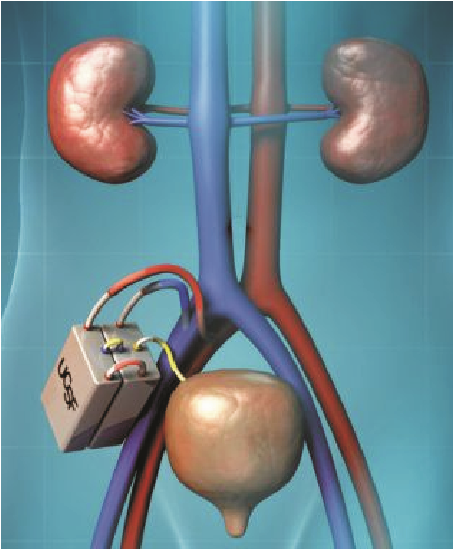
Chronic kidney disease constitutes a public health problem with increasing incidence, prevalence, poor outcomes and high cost. The awareness of and screening for chronic kidney disease remains low worldwide. Thus millions of people around the world suffer from kidney diseases, and these patients eventually will require a form of renal replacement therapy. Outcomes include kidney failure and complications of decreased kidney function with attendant cardiovascular diseases. Dialysis and transplantation, while effective, are not optimal therapies for kidney failure. This is a major reason why researchers have been working on better alternatives including growing 'new kidneys' and creating bioartificial kidney (Kidney Project), to treat end stage renal disease. The Kidney Project1 is a US national research project with a goal to create a small, surgically implanted, bioartificial kidney to treat end stage renal disease (ESRD). The research team is headed by Shuvo Roy, PhD, a bioengineer in the University of California, San Francisco (UCSF), and co-directed by William Fissell, MD, at the Vanderbilt University Medical Center. The bioartificial kidney is expected to save lives and reduce drastically budget committed to renal replacement therapy. After more than 20 years of work, the clinical trials are scheduled to hold early 2018. Although kidney transplantation is still one of the best treatment options of ESRD, unfortunately there is shortage of organ donors that prevents transplants from being available to the vast majority of ESRD patients. Unlike transplants, the bioartificial kidney will not require that patients are on immunosuppressive drugs to prevent rejection2. It will be powered by the body's own blood pressure, and does not require external tubes or tethers2. Accordingly to the lead researcher, 'The implantable bioartificial kidney builds upon the existing extracorporeal Renal Assist Device (RAD), which is a bioartificial kidney that combines a membrane hemofilter and a bioreactor of human renal tubule cells to mimic many of the metabolic, endocrine, and immunological functions of a healthy kidney. While clinical trials confirmed that the RAD can safely treat acute renal failure in a critical care setting, adoption of the RAD for routine treatment of ESRD patients is hampered by its labor-intensive and complex operation, large size, and high marginal cost. The ultimate goal of The Kidney Project is to apply micro-electromechanical systems (MEMS) and nanotechnology to miniaturize the extracorporeal RAD into a surgically implantable, self-monitoring, and self-regulating bioartificial kidney.'
References
https://www.wired.com/story/artificial-kidneys/
M. Takasato, P. X. Er, M. Becroft, J. M. Vanslambrouck, E. G. Stanley, A. G. Elefanty et al. Directing human embryonic stem cell differentiation towards a renal lineage generates a self-organizing kidney. Nature Cell Biology 16, 118-126, 2014
Cell, Wu et al.: "Interspecies chimerism with mammalian pluripotent stem cells." www.cell.com/cell/fulltext/S00928674(16)31752-4. DOI: 10.1016/j.cell.2016.12.036
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Research Journal of Health Sciences

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Research Journal of Health Sciences journal is a peer reviewed, Open Access journal. The Journal subscribed to terms and conditions of Open Access publication. Articles are distributed under the terms of Creative Commons License (CC BY-NC-ND 4.0). (http://creativecommons.org/licences/by-nc-nd/4.0). All articles are made freely accessible for everyone to read, download, copy and distribute as long as appropriate credit is given and the new creations are licensed under the identical terms.

