Anatomy of lead poisoning
Keywords:
Lead poisoning, anatomy, cellular pathways, trace elementsAbstract
Objective: Lead poisoning and lead toxicity is usually often interchangeably used by different Scientists. The Anatomy of lead poisoning encompasses its effects on different organ-systems of different species of organisms. It also includes environmental, functional and biochemical components associated with most heavy metals that enters biological tissues daily through occupational and environmental exposures. A major outbreak of lead poisoning occurred in Zamfara state Nigeria in 2010, killing over 500 children. Also inMay 2015, Niger state Nigeria was plagued with another outbreak and children were the most affected.Mining activities have increased, oil exploration and pipeline vandalism, have destroyed our ecosystems just to mention a few of the factors responsible for unabated increased levels of heavy metals in our bodies resulting into congenital malformations, infertility, reduced intelligent quotient in children, and cancer.
Methods: Different literature in reputable journals were reviewed in the course of this study. New mechanisms involved in the toxicity of heavy metals were studied. Advances in molecular biology have however tremendously helped in unravelling more mechanisms of lead toxicity.
In this review it is perceived that a population of males or females may surfer adverse reproductive sequelae in future.
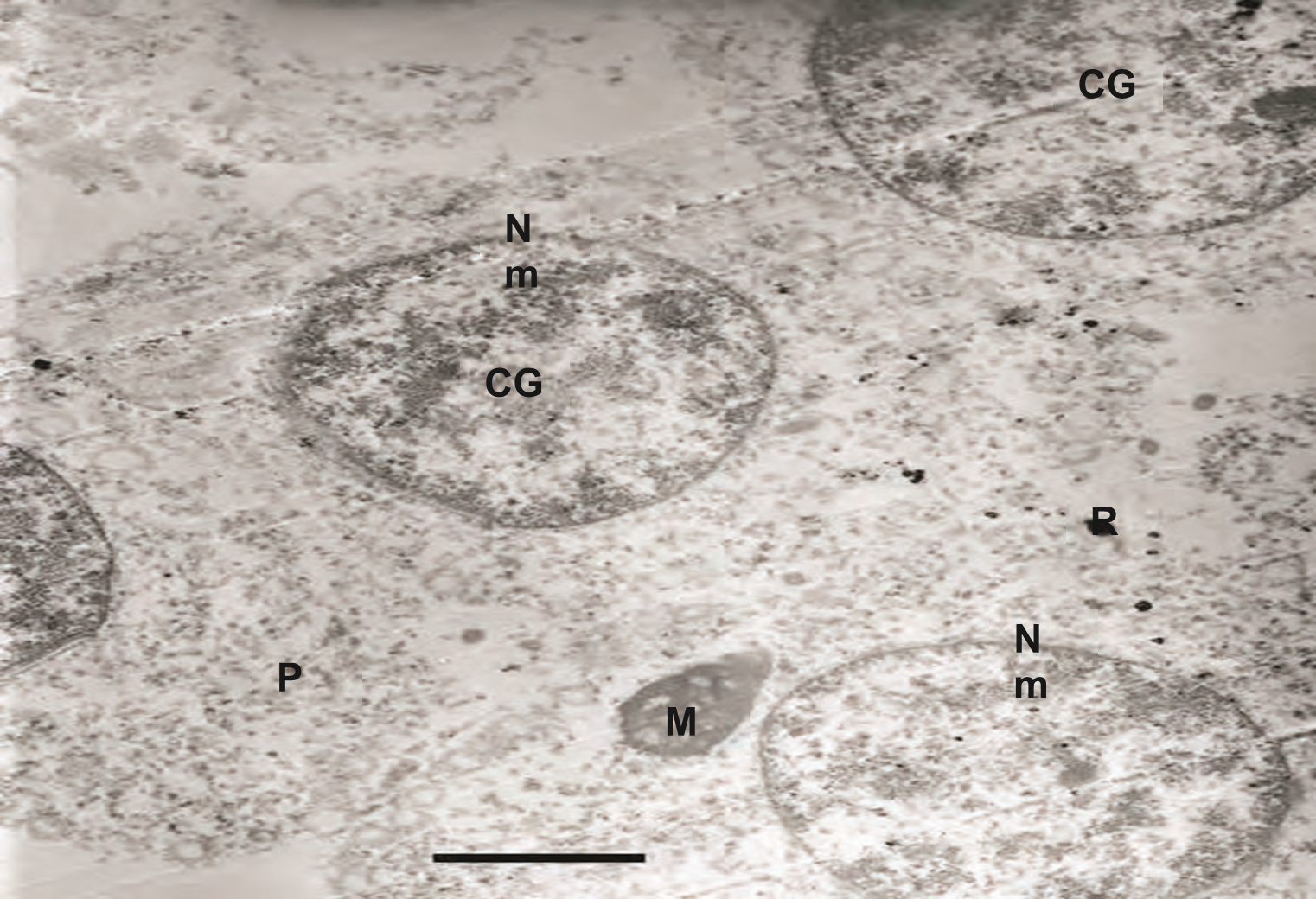
Results: The primary form of lead toxicity is by oxidative stress mechanisms, apoptosis and necrosis involving cellular pathways including both mitochondria and cytoplasmic pathways.
Conclusions: Lead and heavy metal toxicities can be ameliorated by synergistic activity of trace elements including selenium, cobalt, zinc and boron.
References
Brake A, Krause W. Decreasing quality of semen. BMJ 1992; 305: 1498
Lewis SE, Aitken RJ. DNA damage to spermatozoa has impacts on
fertilization and pregnancy. Cell Tissue Res 2005; 322: 33–41.
Olsen GW, Bodner KM, Ramlow JM, Ross CE, Lipshultz LI. Have sperm counts been reduced 50 percent in 50 years? A statistical model revisited. Fertil Steril 1995; 63: 887–93.
Fisch H, Goluboff ET, Olson JH, Feldshuh J, Broder SJ, Barad DH. Semen analyses in 1 283 men from the United States over a 25-year period: No decline in quality. Fertil Steril 1996; 65: 1009–14.
Parvinen M, Lahdetie J, Parvinen LM. Toxic and mutagenic influences on spermatogenesis. Arch Toxicol Suppl 1984; 7: 128–39.
Niederberger C. Exposure to persistent organochlorine pollutants associates with human sperm Y:X chromosome ratio. Hum Reprod 2005; 20: 1903–9.
Guillette LJ Jr, Gross TS, Masson GR, Matter JM, Percival HF, Woodward
AR. Developmental abnormalities of the gonad and abnormal sex hormone concentrations in juvenile alligators from contaminated and control lakes in Florida. Environ Health Perspect 1994; 102: 680–8
Kavlock RJ, Perreault SD. Multiple chemical exposure and risks of adverse reproductive function and outcome. In: Toxicological of Chemical
Mixtures: From Real Life Examples to
Mechanisms of Toxicology
Interactions. Yang RS, editor. Academic Press: Orlando. 1994; p245–97.
Sokol RZ. Hormonal effects of lead acetate in the male rat: mechanism of action. Biol Reprod 1987; 37: 1135–8.
Sikka SC. Gonadotoxicity. In: Male Infertility and Sexual Dysfunction.
Hellstrom WJ, editor. SpringerVeerlag, New York. 1997; p292–306.
Lamb DJ. Hormonal disruptors and male infertility: are men at serious risk? Regul Toxicol Pharmacol 1997; 26: 30–3. 12 Cheek AO, McLachlan JA. Environmental hormones and the male reproductive system. J Androl 1998; 19: 5–10. 13 McLachlan JA, Arnold SF. Environmental estrogens. Amer Sci 1996; 84: 452–61.
Cheek AO, McLachlan JA.
Environmental hormones and the male reproductive system. J Androl 1998; 19: 5–10. 13 McLachlan JA, Arnold SF. Environmental estrogens. Amer Sci 1996; 84: 452–61.
Colborn T, vomSaal FS, Soto AM. Developmental effects of endocrinedisrupting chemicals in wildlife and humans. Env Health Prospect 1993; 1101: 378–84.
Sikka SC, Nigun G. Reproductive Toxicity of Organophosphate and Carbamate Pesticides. In: Toxicology of Organophosphate and Carbamate Compounds. Gupta RC, editor.
Elsevier Academic Press: New York. 2005; Chapter 32, p447–62.
Kelce WR, Monosson E, Gamcsik MP, Laws SC, Gray LE Jr. Environmental hormone disruptors: evidence that vinclozolin developmental toxicity is mediated by antiandrogenic
metabolites. Toxicol Appl Pharm 1994; 126: 276–85.
Sharpe RM, Skakkebaek NE. Are estrogens involved in falling sperm counts and disorders of the male reproductive tract? Lancet 1993; 351: 1392–5.
Working PK. Male reproductive toxicology: comparison of the human to animal models. Environ Health Prospect 1988; 77: 37–44.
Sokol RZ. Toxicants and infertility: identification and prevention. In: Management of impotence and infertility. Whitehead ED, Nagler HM, editors. JB Lippincott Company: Philadelphia. 1994; p380–9.
Angelopoulou R, Plastira K, Msaouel P. Spermatozoal sensitive biomarkers to defective protaminosis and fragmented DNA. Reprod Biol
Endocrinol 2007; 5: 36.
Mandl AM. The radiosensitivity of germ cells. Biol Rev Camb Philos Soc 1964; 39: 288–371.
Whorton D, Krauss RM, Marshall S,
Milby TH. Infertility in male pesticide workers. Lancet 1977; 2: 1259–61.
Mattison DR. The mechanisms of action of reproductive toxins. Am J Ind Med 1983; 4: 65–79. Potashnik G, Yanai-Inbar I. Dibromochloropropane (DBCP): an 8-year reevaluation of testicular function and reproductive performance. Fertil Steril 1987; 47: 317–23.
Kelce WR, Stone CR, Laws SC, Gray LE, Kemppainen JA, Wilson EM. Persistent DDT metabolite p,p'-DDE is
a potent androgen receptor antagonist. Nature 1995; 375: 581–5.
Vine MF, Tse CK, Hu P, Truong KY. Cigarette smoking and semen quality. Fertil Steril 1996; 65: 835–42.
Schrader SM. Principles of male reproductive toxicology. In: Environmental Medicine. Brooks SM, Gochfeld M, editors. St. Louis: Mosby Press. 1995; p95–100.
Gilfillan SC. Lead poisoning and the fall of Rome. J Occup Med 1965; 7: 53–60.
Lancranjan I, Popescu HI, Gavanescu O, Klepsch I, Serbanescu M. Reproductive ability of workmen occupationally exposed to lead. Arch Environ Health 1975; 30: 396–401-30.
Gilfillan SC. Lead poisoning and the fall of Rome. J Occup Med 1965; 7: 53–60Winder C. Reproductive and chromosomal effects of occupational exposure to lead in males. Reprod Toxicol 1989; 3: 221–33.
Ewing LL, Zirkin BR, Chubb C.
Assessment of testicular testosterone production and Leydig cell structure. Environ Health Perspect 1981; 38: 19–27.
Foster WG, McMahon A,Young-Lai EV, Hughes EG, Rice DC.
Reproductive endocrine effects of chronic lead exposure in the male cynomolgus monkey. Reprod Toxicol 1993; 7: 203–9.
Braunstein GD, Dahlgren J, Loriaux DO. Hypogonadism in chronically lead poisoned men. Infertility 1978; 1: 33–51.
Weir RJ Jr, Fisher RS. Toxicological studies on borox and boric acid.
Toxicol Appl Pharmacol 1972; 23: 351–64.
Friberg L, Piscator M, Nordberg GF. Cadmium in the environment, 2nd edition. Cleveland: CRC Press Inc.. 1974; p37–53.
Falana BA, Odundele OM, Duru FI, Osinubi AA, Falode DT (2013).
Molecular Characterization of
Alkaline Phosphatase and PLAP in the Germinal Epithelium of Pb and Se+Zn Treated Adult Sprague-Dawley Rats.
Cell & Developmental Biology
/2013; 2(3):1-4.
King LM, Anderson MG, Sikka SC,
George WJ. Murine strain differences in cadmium-induced testicular toxicity. Arch Toxical 1998; 72: 650–5.
Snow ET. Metal carcinogenesis: mechanistic implications. Pharmacol
Ther 1992; 53: 31–65
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Research Journal of Health Sciences

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Research Journal of Health Sciences journal is a peer reviewed, Open Access journal. The Journal subscribed to terms and conditions of Open Access publication. Articles are distributed under the terms of Creative Commons License (CC BY-NC-ND 4.0). (http://creativecommons.org/licences/by-nc-nd/4.0). All articles are made freely accessible for everyone to read, download, copy and distribute as long as appropriate credit is given and the new creations are licensed under the identical terms.

