Hypogonadism among obese type 2 diabetic men in South-Western Nigeria
Keywords:
Hypogonadism, obesity, FSH, LH, testosterone, NigeriaAbstract
Background: Studies have shown that hypogonadism is closely related to the development of Type 2 Diabetes. This study aimed to assess hypogonadism among type 2 diabetic and obese male patients in Southwest Nigeria.
Methods: One hundred and twenty men consisting of thirty obese diabetics, thirty non-obese diabetics, thirty obese non-diabetics and thirty non-obese non-diabetics, were included in the study. Participants were interviewed to obtain data on biodata, reproductive characteristics, and anthropometry. Venous Blood was collected for the determination of fasting plasma Glucose, glycated haemoglobin, and reproductive hormonal levels.
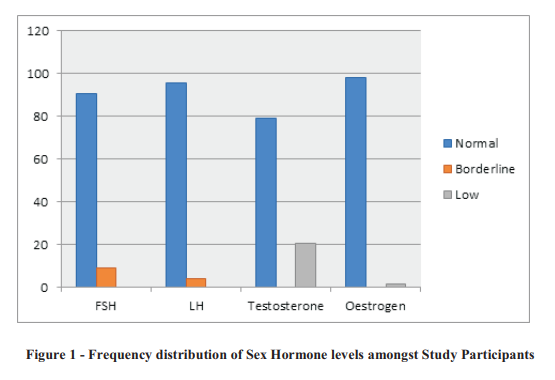
Results: The prevalence of hypogonadism in this study was 20.8%. The mean age of all the participants was 43.39 ± 5.21, most men being in the 40-44 years age group. In this age group, over a third (40%) of the men had low testosterone. Out of the 60 participants who were diabetic, 18 (30%) had low testosterone, two-third of whom (66.7%) were obese. Mean testosterone was significantly lower in obese diabetics when compared with non-obese diabetics. The mean testosterone and FSH were significantly lower in obese non-diabetics as well. Both diabetic and non-diabetic groups had significantly higher estrogen in the obese participants, than in the non-obese.
Conclusion: In conclusion, hypogonadism is a common finding among diabetic men, and it occurs in higher frequency with coexisting obesity. Hence, a holistic approach in the treatment of male patients with hypogonadism, type 2 diabetics and obesity should be considered, in order to safeguard their reproductive health.
References
World Health Organization. Diabetes [Internet]. 2018 [cited 2018 Dec 5]. Available from: http://www.who.int/news-room/fact-
sheets/detail/diabetes
Association AD. Diagnosis and classification of diabetes mellitus. Vol. 33, Diabetes Care. American Diabetes Association; 2010. p. S62.
Zheng R, Cao L, Cao W, Chu X, Hu Y, Zhang H, et al. Risk Factors for Hypogonadism in Male Patients with Type 2 Diabetes. J Diabetes Res. 2016;2016.
McBride JA, Carson CC, Coward RM.
Testosterone deficiency in the aging male. Ther Adv Urol [Internet]. 2016 Feb 5 [cited 2020 Apr
] ; 8 ( 1 ) : 4 7 – 6 0 . Av a i l a b l e f r o m :
http://www.ncbi.nlm.nih.gov/pubmed/26834840
Livshits A, Seidman DS. Fertility issues in women with diabetes. Vol. 5, Women's Health. Womens Health (Lond); 2009. p. 701–7.
Ding GL, Liu Y, Liu ME, Pan JX, Guo MX, Sheng JZ, et al. The effects of diabetes on male fertility a n d e p i g e n e t i c r e g u l a t i o n d u r i n g
spermatogenesis. Vol. 17, Asian Journal of Andrology. Medknow Publications; 2015. p. 948–53.
Betancourt-Albrecht M, Cunningham G. Hypogonadism and Diabetes. Int J Impot Res. 2003;15:514–20.
Holt S, Lopushnyan N, Hotaling J, Sarma A, Dunn R, Cleary P, et al. Prevalence of low testosterone and predisposing risk factors in men with type 1diabetes mellitus: findings from the
DCCT/EDIC. J Clin Endocrinol Metab. 2014;99:E1655–E1660.
Al Hayek A, Ajlouni K, Khader Y, Jafal S, Khawaja N, Robert A. Prevalence of low testosterone levels in men with type 2 diabetes mellitus: a cross-sectional study. J Fam Community Med. 2013;20(3):179.
Traish AM, Feeley RJ, Guay A. Mechanisms of obesity and related pathologies: Androgen deficiency and endothelial dysfunction may be the link between obesity and erectile dysfunction. Vol. 276, FEBS Journal. FEBS J; 2009. p. 5755–67.
Allan CA, McLachlan RI. Androgens and obesity. Vol. 17, Current Opinion in Endocrinology, Diabetes and Obesity. Curr Opin Endocrinol Diabetes Obes; 2010. p. 224–32.
Brand J, Van derTweel I, Grobbee D, EmmelotVonk M, Van der Schouw Y. Testosterone, Sex Hormone-Binding Globulin and the Metabolic
Syndrome: A Systematic Review and MetaAnalysis of Observational Studies. Int J
Epidemiol [Internet]. 2011 [cited 2020 Apr 3];40(1):189–207. Available from:
https://academic.oup.com/ije/article/40/1/189/6
Sexton WJ, Jarow JP. Effect of diabetes mellitus upon male reproductive function. Vol. 49, Urology. Urology; 1997. p. 508–13.
Fedele D. Therapy insight: Sexual and bladder dysfunction associated with diabetes mellitus. Vol. 2, Nature Clinical Practice Urology. Nat Clin Pract Urol; 2005. p. 282–90.
Kolodny R, Khan C, Goldstein H, Barnett D. Sexual dysfunction in diabetic men,. Diabetes. 1974;23:306–9.
Kim MJ, Rolland Y, Cepeda O, Gammack JK, Morley JE. Diabetes mellitus in older men. Vol. 9, Aging Male. Taylor & Francis; 2006. p. 139–47.
Cochran W. Sampling techniques. 3rd editio. New York: John Wiley and Sons; 1977.
Akinjimi A, Adeyooye O, Akingbade O,
Okerentugba P. Prevalence of Diabetes Mellitus in Abeokuta, Ogun state, Nigeria. Researcher. 2014;6(2):73–5.
Dandona P, Dhindsa S, Chande A, Topiwale S. Low testosterone in men with type 2 diabetes – a growing public health concern. Diabetes Voice. 2009;54(2).
World Health Organization MC. Overweight and Obese: BMI classification. Available from: http://www.who.int/bmi/index.jsp?introPage=in tro_3.html
Surampudi PN, Wang C, Swerdloff R. Hypogonadism in the aging male diagnosis, potential benefits, and risks of testosterone replacement therapy. Int J Endocrinol. 2012;2012.
Mulligan T, Frick MF, Zuraw QC, Stemhagen A, McWhirter C. Prevalence of hypogonadism in males aged at least 45 years: The HIM study. Int J Clin Pract. 2006 Jul;60(7):762–9.
Dhindsa S, Ghanim H, Batra M, Dandona P. Hypogonadotropic hypogonadism in men with diabesity. Vol. 41, Diabetes Care. American Diabetes Association Inc.; 2018. p. 1516–25.
Dhindsa S, Furlanetto R, Vora M, Ghanim H, Chaudhuri A, Dandona P. Low estradiol concentrations in men with subnormal testosterone concentrations and type 2 diabetes. Diabetes Care. 2011 Aug 1;34(8):1854–9.
Loves S, Ruinemans-Koerts J, de Boer H. Letrozole once a week normalizes serum testosterone in obesity-related male hypogonadism. Eur J Endocrinol. 2008 May;158(5):741–7.
Guzik T, D M, Korbut R. Adipo-cytokines: novel link between inflammation and vascular function? J Pharmacol. 2006;57:505–28.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Research Journal of Health Sciences

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Research Journal of Health Sciences journal is a peer reviewed, Open Access journal. The Journal subscribed to terms and conditions of Open Access publication. Articles are distributed under the terms of Creative Commons License (CC BY-NC-ND 4.0). (http://creativecommons.org/licences/by-nc-nd/4.0). All articles are made freely accessible for everyone to read, download, copy and distribute as long as appropriate credit is given and the new creations are licensed under the identical terms.

