An audit of uterovaginal prolapse in Ogbomoso, south-west Nigeria.
Keywords:
Difficult labour, uterovaginal prolapse, hysterectomy, multiparityAbstract
Objective: Uterovaginal prolapse (UVP) as a gynaecological problem is very common especially in multipara. This condition is important to gynaecologists practicing in Sub-Saharan Africa because of its strong link with multiparity, poor conduct of labour, and most importantly, its role as a cause of chronic morbidity in many post-menopausal women necessitating major gynaecological surgeries..
Methods: A retrospective study of utero-vaginal prolapse to determine the prevalence, presentation , management patterns and complications of UVP at the Bowen University Teaching Hospital , Ogbomosho, Oyo State, Nigeria between January 1, 2010 and December 31, 2014. Relevant data were obtained from the case notes, which included age, parity, presenting symptoms, number of living children, types of delivery, types of surgical management and associated operative morbidity and mortality. The data were presented as simple percentages.
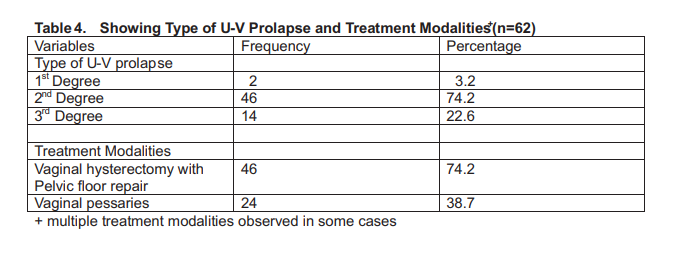
Results : The prevalence of uterovaginal prolapse was 5.4%. The mean age at presentation was 51.4± 3.3 years. The mean parity was 4.2± 1.6. Fifty-six (90.3%) of them were at least 40 years old . Majority of the patients( 80.6%) were grand-multiparous. The commonest symptom was 'something coming down the vagina' in 96% of the study subjects. Difficult labour was found to be the most common associated factor in 47 (76.2%) of the patients Second degree prolapse was the commonest type of presentation (74.2%). The most common form of treatment offered was vaginal hysterectomy with pelvic floor repair, 46 (74.2%) of the patients. Twenty -four (38.7%) patients had vaginal pessaries inserted for various degrees of UVP.
Conclusion: Uterovaginal prolapse is a common gynaecological condition of the parous and elderly postmenopausal women associated with a decreased body image and quality of life. Supervised hospital deliveries and limiting the family size by efficient contraception deserve priority attention to prevent this social malady.
References
Tarney CM, Dorr CH: Relaxation of Pelvic Support In: DeCherney AH, Nathan L (eds) Current Obstetric and Gynecological Diagnosis
and Treatment, 9th Edition. New York McGrawHill Companies 2003; 776-797.
Robinson D. Urogenital Prolapse, In: Luesley DM, Baker PN (eds). Obstetrics and
Gyaecology: An evidence-based text for MRCOG 1st Edition London, Anorld 2004; 661670.
John CT. Genital Prolapse. In: Okonofua FE,
Odunsi K (eds) Contemporary Obstetrics and Gynaecology for Developing Countries. Benin City, WHARC 2003; 214-226.
Stanton SL. Vaginal Prolapse. In: Edmonds DK (ed) Dewhurt's Textbook of Obstetrics and Gynaecology for Post graduates, 6th Edition: London, Blackwell Science 1999; 462-473
Jeffcoates TNA. Genital prolapse. In: Jeffcoates TNA (Ed). Principles of gynaecology. 7th ed; India, Jaypee; 2008:324-334.
Lewis AC. Major Gynaecology surgery in the elderly. J Int Fed Gynaecol Obstet 1968; 6:244-
Agboola A. Urogenital prolapse and displacement of the uterus. In: Agboola A (Ed). Textbook of obstetrics and gynaecology for medical students, 2nd ed; Ibadan, Heinemann Educational Books (Nig) Plc; 2006: 31-39.
Smi ARB. Pelvic floor dysfunction 1: uterovaginal prolapse. In: Edmonds DK (Ed). Dewhurst's Textbook of Obstetrics and Gynaecology; 7th ed; Oxford, Blackwell Publishing; 2007:496-503.
Tindall VR. Genital prolapse. In: Tindall VR. (Ed). Jeffcoates principle of gynaecology. 5thed. London, Butterworths and Co. Publishers; 1987:260-274.
O' Leary JA, O' Laery JL. The extended Manchester operation: A review of 289 cases. Am J Obstet Gynecol 1990; 107:564-559.
P. Pelvic Kushtagi Organ Prolapse. In: Arulkumaran S, Sivanesaratnam V, Chatterjee A, Kumar P (Eds). Essentials of Gynaecology;
New Delhi, Jaypee Brothers Medical
Publishers; 2005:147-155
Okonkwo JE, Obiechina NJ, Obionu CN.
Incidence of pelvic organ prolapse in Nigerian women. J Nath Med Assoc. 2003; 95(2):132136.
Balogun OR. Genital Prolapse in Ilorin: A-seven year review. Niger J Med 1997: 6(3):77-82.
Onowhakpor EA, Omo-Aghoja LO, Akani CI, Feyi-Waboso P. Prevalence and determinants of uterovaginal prolapse in Southern Nigeria. Niger Med J. 2009; 50(2): 29-32.
Omolayole JA, Akingba JB. Procidential in adolescence. Niger Med J. 1975; 5: 277-279
Osinusi BO, Adeleye JA. The symptomatology and clinical presentation of uterovaginal prolapse in Ibadan. Niger Med J 1976; 8:451-
Ogunbode O, Aimakhu VE. Uterine proplapse during pregnancy in Ibadan. Am J Obstet Gynaecol 1973; 16:622-625.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Research Journal of Health Sciences

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Research Journal of Health Sciences journal is a peer reviewed, Open Access journal. The Journal subscribed to terms and conditions of Open Access publication. Articles are distributed under the terms of Creative Commons License (CC BY-NC-ND 4.0). (http://creativecommons.org/licences/by-nc-nd/4.0). All articles are made freely accessible for everyone to read, download, copy and distribute as long as appropriate credit is given and the new creations are licensed under the identical terms.

