Prevalence, predictors, and perceived susceptibility to placental malaria parasitemia among pregnant women in a tertiary hospital in South-Western Nigeria
Keywords:
Prevalence,, risk factors, placental malaria, pregnancyAbstract
Objective: Is to determine the prevalence and predictors of placental malaria among pregnant women.
Methodology: The study was cross-sectional in design. It was carried out over six months. We administered Pretested questionnaire to 300 eligible subjects. The researchers took maternal peripheral blood for malaria parasites while cord and placental blood sample at delivery for neonatal packed cell volume (PCV) and Malaria parasite. Data were analyzed using STATA 10.
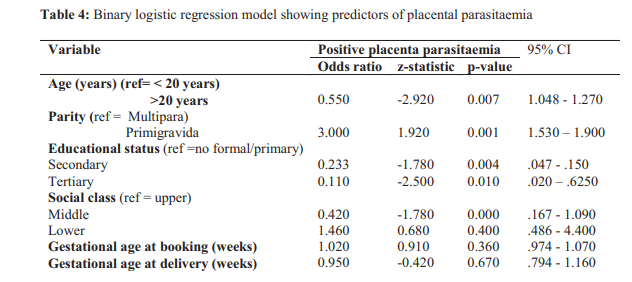
Result: One hundred and forty-four (48%) participants had placental malaria parasitemia, while 173 (57.7%) had peripheral malaria parasitemia. Maternal age less than 20 years (P=0.008), low parity, and hemoglobin type AA (P=0.002) were significantly associated with a higher prevalence of placental parasitemia. Maternal secondary and tertiary education (P=0.013), perceived susceptibility to placental malaria and IPT use (p=0.014) were significantly associated with lower prevalence.
Conclusion: This study has shown that placental parasitemia is a significant problem in pregnancy as it is strongly associated with certain maternal factors. There is the need to intensify control efforts aimed at reducing malaria in pregnancy in Nigeria, and mothers with increased risk factors should receive more focused attention.
References
Durojaye OA, Ilo CC, Okeowhor D, Iyaji RO, Onuorah O, James PO, Cosmas S. The Malaria Concept in Pregnancy and the Mechanism of Evading the Immune System by the Malaria Parasite. South Asian Journal of Parasitology. 2019 Jan 19:1-7.
Iyare FE, Uneke CJ. Effects of placental malaria on placental and neonatal birth weight of primigravidae in Southeastern Nigeria. Nigerian Journal of Experimental and Clinical Biosciences. 2018 Jul 1;6(2):59.
Olawale AN, Donaldson EI. On-Time Domain Analysis of Malaria Morbidity in Nigeria. American Journal of Applied Mathematics and Statistics. 2018;6(4):170-5.
Adeogun AO. Insecticide Resistance Associated
With 2la Inversion And Microsatellite Loci Polymorphism In Anopheles gambiae Ss Populations From Lagos And the Oyo States, Nigeria (Doctoral Dissertation).
Mokuolu OA, Falade CO, Orogade AA, Okafor HU, Adedoyin OT, Oguonu TA, Dada-Adegbola HO, Oguntayo OA, Ernest SK, Hamer DH,
Callahan MV. Malaria at parturition in Nigeria: current status and delivery outcome. Infectious Diseases in Obstetrics and Gynecology. 2009;2009.
Okonofua FE, Adeniran M, Adetugbo D, Nganwuchu A. Prevalence of malaria in women attending the antenatal clinic of Obafemi Awolowo University Teaching Hospital, Ile-Ife Nigeria. Medicare 1990;25:8-11
Tako EA, Zhou A, Lohoue J, Leke R, Taylor DW, Leke RF. Risk factors for placental malaria and its effect on pregnancy outcome in Yaoundé,
C a m e r o o n . A m J Tr o p M e d H y g .
;72:236–242.
Fried M, Duffy PE. Malaria during pregnancy. Cold Spring Harbor perspectives in medicine. 2017 Jun 1;7(6):a025551.
Fehintola AO, Fehintola FO, Loto OM, Fasubaa OB, Bakare B, Ogundele O. Pregnancy and fetal outcome of placental malaria parasitemia in IleIfe, Nigeria. Tropical Journal of Obstetrics and Gynaecology. 2016 Sep 1;33(3):310.
Dawaki S, Al-Mekhlafi HM, Ithoi I, Ibrahim J, Atroosh WM, Abdulsalam AM, Sady H, Elyana FN, Adamu AU, Yelwa SI, Ahmed A. Is Nigeria winning the battle against malaria? Prevalence, risk factors, and KAP assessment among Hausa communities in Kano State. Malaria journal. 2016 Dec;15(1):351.
Iyare FE, Uneke CJ. Effect of placental malaria on placental and neonatal birth weight of primigravidae in Southeastern Nigeria. Nigerian Journal of Experimental and Clinical Biosciences. 2018 Jul 1;6(2):59.
Izuka EO, Ugwu EO, Obi SN, Ozumba BC, Nwagha TU, Obiora-Izuka CE. Prevalence and predictors of placental malaria in human immunodeficiency virus-positive women in Nigeria. Nigerian Journal of clinical practice. 2017;20(1):31-6.
Oweisi PW, John CT, Omietimi JE, Aigere EO, Allagoa DO, Kotingo EL. Placental Malaria Parasitization at Delivery: Experience at a Nigerian Tertiary Hospital. European Scientific Journal, ESJ. 2018 Mar 31;14(9):243..
Umeobika JC, Uzoma MJ, Ojiyi EC, Ikeako LC, Ezenyeaku CT, Ezebialu IU. The Prevalence And Correlation of Placental Malaria Parasitaemia with Neonatal Malaria and Anaemia in Orlu, South-East Nigeria. Tropical Journal of Medical and Health Science Research. 2018 Apr 18;6(1).
Fana SA, Bunza MD, Anka SA, Imam AU, Nataala SU. Prevalence and risk factors associated with malaria infection among pregnant women in a semi-urban community of northwestern Nigeria. Infectious diseases of poverty. 2015 Dec;4(1):24.
Obiajunwa PO, Owa JA, and Adeodu OO,
“Prevalence of congenital malaria in Ile-Ife, Nigeria,” J of Trop ped, vol. 51, no. 4, pp. 219-222, 2005.
Research methodology with statistics for health and social sciences by Margaret Olabisi Araoye. Pp 177 – 122, 2004 edition.
O. Olusanya, E. Okpere, and M. Ezimokhai, “The importance of social class in-voluntary fertility control in a developing country,” West Afr J Med, vol. 4, pp. 205– 211, 1985
Ogbodo CE, Mary JY, Barro D, Cot M. Is malarial placental infection related to a peripheral infection at any time of pregnancy? Am J Trop Med Hyg. 2005;73:1112–1118.
Falade CO, Mokuolu OA, Okafor HU, et al., “Epidemic of congenital malaria in Nigeria: a multi-center study," Trop Med Int Health, vol. 12, no.11, pp. 1279-1287, 2007.
Akinboro RA, Ojurongbe O, Akindele AA, Adefioye OA, Bolaji OS, Olaniran O, Adeyeba OA. Plasmodium falciparum parasitemia in pregnancy in relation to maternal anemia. African
Journal of Clinical and Experimental
Microbiology. 2010;11(3) pp 164-169.
Shuaib F, Jolly P. Socio-demographic determinants of malaria in pregnancy. How well do parents in the United States report heights and weights for children?. 2017 Mar 28:17.
Ugboaja JO, Oguejiofor CO. Efficacy of intermittent preventive treatment and insecticidetreated nets on malaria parasitemia in pregnancy among Igbo women in southeastern Nigeria. Journal of vector-borne diseases. 2017 Jul 1;54(3):249.
Eastman RT, Fidock DA. Artemisinin-based combination therapies: a vital tool in efforts to eliminate malaria. Nature Reviews Microbiology. 2009 Dec;7(12):864.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Research Journal of Health Sciences

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Research Journal of Health Sciences journal is a peer reviewed, Open Access journal. The Journal subscribed to terms and conditions of Open Access publication. Articles are distributed under the terms of Creative Commons License (CC BY-NC-ND 4.0). (http://creativecommons.org/licences/by-nc-nd/4.0). All articles are made freely accessible for everyone to read, download, copy and distribute as long as appropriate credit is given and the new creations are licensed under the identical terms.

