Male Reproductive Complications of Diabetes Mellitus and Possible Medicinal Plant Remedies: A Review.
Keywords:
Diabetes, Complications, Medicinal Plants, Erectile dysfunction, RemediesAbstract
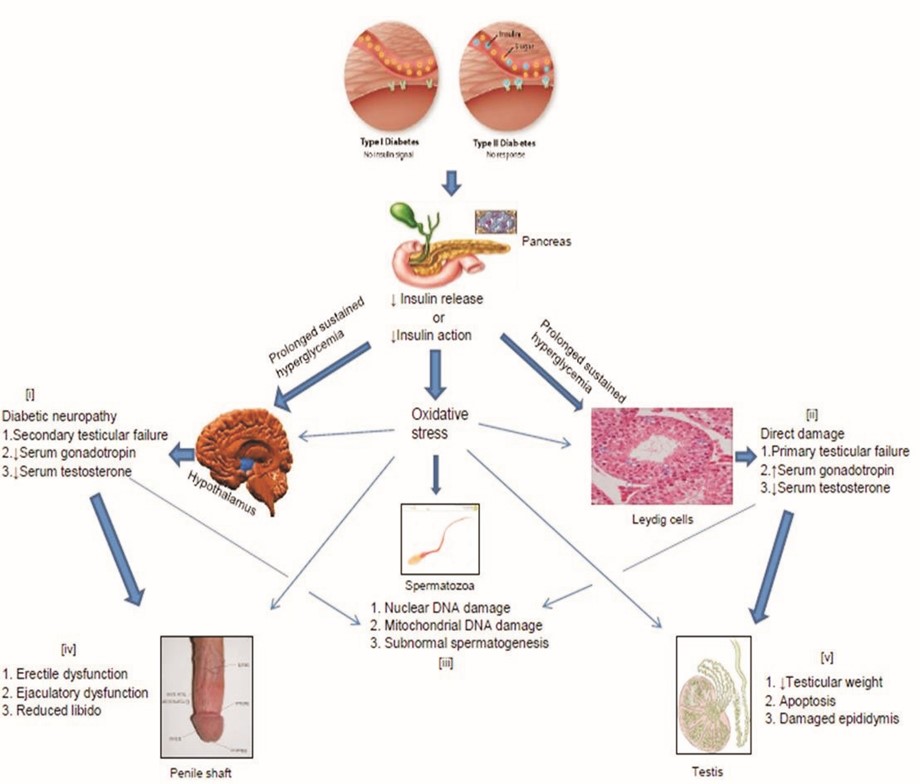
Objective: Male reproductive dysfunction and subsequent infertility are major complications that are becoming increasingly associated with Diabetes Mellitus (DM). Due to frequent failure in treatment with orthodox antidiabetic drugs, there has been a massive shift of attention to alternative therapies. The antidiabetic potential of a large number of medicinal plants have been investigated both in-vitro and in experimental animal models. These specific plants were predominantly used because of the antioxidant capacity of their bioactive phytoconstituents. This review focuses on reproductive dysfunctions commonly suffered by male diabetic patients and medicinal plants that have been tested and reported for their roles in ameliorating such dysfunctions.
Method: All original journal articles and reviews cited on PubMed between 2005 and 2015 in English language were considered for this review.
Results and conclusion: This review reestablished the fact that male infertility is a common complication of poorly managed diabetes mellitus. It also highlighted the fact that the numerous challenges associated with the use of orthodox drugs in management of the disease makes medicinal plant therapy inevitable. However, the full potentials of these medicinal plants at correcting reproductive complications of the disease are still to be realized and more specific studies are required in this field for improved therapeutic outcomes.
References
American Diabetic Association. Diabetes care 2012; 35(1): s64-s75.
Jain GC, Jangir RN. Modulation of diabetesmellitus-induced male reproductive dysfunctions in experimental animal models with medicinal plants. Pharmacogn Rev. 2014; 8(16): 113-121.
Mallidis C, Agbaje I, McClure N, Kliesch S. The influence of diabetes mellitus on male reproductive function: A poorly investigated aspect of male infertility. Urologe. 2011; 50(1): 33-7.
La Vignera S, Condorelli R, Vicari E, D'agata R, Calogero AE. Diabetes mellitus and sperm parameters. J. Androl. 2012; 33 (2): 145-153.
Agbaje IM, Rogers DA, McClure CM, Atkinson AB, Mallidis C, Lewis SEM . Insulin dependent diabetes mellitus: Implications for male reproductive function. Hum Reprod. 2007; 22(7): 1871-1877.
Abdolahnejad A, Gol A, Dabiri S. Garlic effects on reproductive complications of diabetes mellitus in male rats. Physiol Pharmacol. 2009; 13(3): 297-307.
Wankeu-Nya M, Florea A, Balici S, Watcho P, Matei H, Kamanyi A. Dracaena arborea alleviates ultra-structural spermatogenic alterations in streptozotocin-induced diabetic rats. BMC Complement Altern Med. 2013; 13:71.
Long L, Wang J, Lu X, Xu Y, Zheng S, Luo C. Protective Effects of Scutellarin on Type II Diabetes Mellitus-Induced Testicular Damages Related to Reactive Oxygen Species/Bcl-2/Bax a n d R e a c t i v e O x y g e n
Species/Microcirculation/Staving Pathway in Diabetic Rat. J Diabetes Res. 2015;Volume 2015,Article ID 252530: 1-11.
Soudamani S, Malini T, Balasubramanian K. Effects of streptozotocin-diabetes and insulin replacement on the epididymis of prepubertal rats: histological and histomorphometric studies. Endocr Res. 2005; 31(2):81-98.
Mallidis C, Green BD, Rogers D, Agbaje IM,
Hollis J, Migaud M et al. Metabolic profile changes in the testes of mice with streptozotocininduced type 1 diabetes mellitus. International J Androl 2009; 32(2):156-165.
Amaral S, Oliveira PJ, Ramalho-Santos J. Diabetes and the Impairment of Reproductive Function: Possible Role of Mitochondria and Reactive Oxygen Species. Curr Diabetes Rev 2008; 4(1):46-54.
Delfino M, Imbrogno N, Elia J, Capogreco F, Mazzilli F. Prevalence of diabetes mellitus in male partners of infertile couples. Minerva Urol Nefrol 2007; 59:131–135.
Portela JM, Tavares RS, Mota PC, RamalhoSantos J, Amaral S. High glucose concentrations per se do not adversely affect human sperm function in vitro. Reproduction 2015; 150(1):7784.
Scarano WR, Messias AG, Oliva SU, Klinefelter GR, Kempinas WG. Sexual behaviour, sperm quantity and quality after short-term streptozotocin-induced hyperglycaemia in rats. Int J Androl 2006; 29(4):482-488.
Awad H, Salem A, Gadalla A, Abou El Wafa N, Mohamed OA. Erectile function in men with diabetes type 2: Correlation with glycemic control. Int J Impot Res. 2010; 22: 36-39.
Moore CR, Wang R. Pathophysiology and treatment of diabetic erectile dysfunction. Asian J Androl 2006; 8(6): 675-684.
Hackett G, Cole N, Bhartia M, Kennedy D, Raju J, Wilkinson P. Testosterone replacement with long-acting testosterone undecanoate improves sexual function and quality-of-life parameters Vs. placebo in a population of men with type 2 diabetes.J Sex Med 2013; 10(6): 1612-1627.
Musicki B, Kramer MF, Becker RE, Burnett AL. Inactivation of phosphorylated endothelial nitric oxide synthase (Ser-1177) by O -GlcNAc in diabetes-associated erectile dysfunction. PNAS 2005; 102(33): 11870-11875.
Hirata H, Kawamoto K, Kikuno N, Kawakami T, Kawakami K, Saini S et al. Restoring erectile function by antioxidant therapy in diabetic rats. J Urol. 2009; 182(5): 2518-2525.
Zhou F, Li GY, Gao ZZ, Liu J, Liu T, Li W et al. The TGF-â1/Smad/CTGF pathway and corpus cavernosum fibrous-muscular alterations in rats with streptozotocin-induced diabetes. J Androl 2012; 33(4): 651-659.
Pontes DA, Fernandes GSA, Piffer RC, Gerardin DCC, Pereira OCM, Kempinas WG. Ejaculatory dysfunction in streptozotocin-induced diabetic rats: the role of testosterone. Pharmacol Rep 2011; 63: 130-138.
Arafa M, El Tabie O. Medical treatment of retrograde ejaculation in diabetic patients: A hope for spontaneous pregnancy. J sex med 2008; 5(1): 194-198.
Sexton WJ, Jarow JP. Effect of Diabetes Mellitus upon Male Reproductive Function. Urology 1997; 49(4): 508-513.
Schoeller EL, Albanna G, Frolova AI, Moley KH. Insulin rescues impaired spermatogenesis via the hypothalamic-pituitary-gonadal axis in Akita diabetic mice and restores male fertility. Diabetes 2012; 61(7): 1869-1878.
Tirabassi G, Corona G, Lamonica GR, Lenzi A,
Maggi M, Balercia G. Diabetes MellitusAssociated Functional Hypercortisolism Impairs
Sexual Function in Male Late-Onset
Hypogonadism. Horm Metab Res 2015; 47: 9.
Nantia EA, Moundipa PF, Monsees TK, Carreau S. Medicinal plants as potential male antiinfertility agent: A review. Andrologia 2009; 19: 148-158.
Sangameswaran B, Jayakar B. Anti-diabetic, anti-hyperlipidemic and spermatogenic effects of Amaranthus spinosus Linn on streptozotocininduced diabetic rats. J Nat Med 2008; 62: 79-82.
Ghosh A, Jana K, Ali KM, De D, Chatterjee K, Ghosh D. Corrective role of Eugenia Jambolana on testicular impairment in streptozotocininduced diabetic male albino rats: An approach through genomic and proteomic study.
Andrologia 2014; 46: 296-307.
Mallick C, Manda Sl, Barik B, Bhattacharya A, Ghosh D. Protection of Testicular Dysfunctions by MTEC, a Formulated Herbal Drug, in Streptozotocin Induced Diabetic Rat. Biol Pharm Bull 2007; 30(1):84-90.
Khaki A, Fathiazad F, Nour M, Khaki AA,
Maleki NA, Khamnei HJ, et al. Beneficial effects of Quercetin on sperm parameters in
streptozotocin-induced diabetic rats. Phytother Res 2010; 24: 1285-1291.
Shalaby MA, Hamowich AR. Safety and efficacy of Zingiber officinale roots on fertility of male diabetic rats. Food Chem. Toxicol 2010; 48: 2920-2924.
Zhou F, Xin H, Liu T, Li G, Gao Z, Liu J et al. Effects of Icariside II on improving erectile function in rats with streptozotocin-induced diabetes. J Androl 2012; 33(5): 832-844.
Yang J, Wang T, Yang J, Rao K, Zhan Y, Chen R, et al. S-Allyl Cysteine restores erectile function through inhibition of reactive oxygen species generation in diabetic rats. Andrology 2013; 1: 487-494.
Yang R, Wang J, Chen Y, Sun Z, Wang R, Dai Y. Effect of Caffeine on erectile dysfunction via upregulating cavernous cyclic Guanosine monophosphate in diabetic rats. J Androl 2008; 29: 586-591.
Ha US, Koh JS, Kim HS, Woo JC, Kim SJ, Jang H, et al. Cyanidin-3-O-â-D-glucopyranoside concentrated materials from mulberry fruit have a potency to protect erectile function by minimizing oxidative stress in a rat model of diabetic erectile dysfunction. Urol Int 2012; 88(4): 470-6.
Khaki A, Khaki AA, Hajhosseini L, Golzar FS, Ainehchi N. The anti-oxidant effects of Ginger and Cinnamon on spermatogenesis dys-function of diabetic rats. Afr J Tradit Complement Altern Med. 2014; 11(4): 1-8.
Thakur M, Chauhan NS, Sharma V, Dixit VK, Bhargava S. Effect of Curculigo orchioides on hyperglycemia-induced oligospermia and sexual dysfunction in male rats. Int J Impot Res. 2012; 24(1): 31-7.
Nene UA, Coyaji K, Apte H. Infertility: A label of choice in the case of sexually dysfunctional couples. Patient Educ Couns 2005; 59: 234-238.
Penson DF, Latini DM, Lubeck DP, Wallace KL, Henning JM, Lue TF. Do impotent men with diabetes have more severe erectile dysfunction and worse quality of life than the general population of impotent patients?; Results from the exploratory comprehensive evaluation of erectile dysfunction (ExCEED) database. Diabetes care 2003; 26(4): 1093-99.
Oger-Roussel S, Behr-Roussel D, Caisey S, Kergoat M, Charon C, Audet A, et al. Bladder and erectile dysfunctions in the Type 2 diabetic
Goto-Kakizaki rat. Am J Physiol Regul Integr Comp Physiol. 2013; 306: R108-R117.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Research Journal of Health Sciences

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Research Journal of Health Sciences journal is a peer reviewed, Open Access journal. The Journal subscribed to terms and conditions of Open Access publication. Articles are distributed under the terms of Creative Commons License (CC BY-NC-ND 4.0). (http://creativecommons.org/licences/by-nc-nd/4.0). All articles are made freely accessible for everyone to read, download, copy and distribute as long as appropriate credit is given and the new creations are licensed under the identical terms.

