Neurosurgical management of spontaneous intracerebral haematoma in a resource-limited setting: profile and challenges
Keywords:
Spontaneous Intracerebral Haematoma, SICH, stroke, neurosurgery, resource-limited setting, Sub-Saharan AfricaAbstract
Background: Spontaneous inracerebral haematoma (SICH) is the most devastating
type of stroke and challenges of its care in resource-limited settings may worsen its
gloomy outlook. There is a need to provide neurosurgical data for SICH in resourcelimited settings. This study provides information about SICH in such a setting.
Method: We conducted a retrospective review of patients who had neurosurgery for
SICH at the UNIOSUN Teaching Hospital, Osogbo, Nigeria over an eleven year
period (October 2011 to June 2022). Demographics, clinical presentations,
operative procedures and outcomes/challenges of care were reviewed. Descriptive
and inferential data analyses were performed.
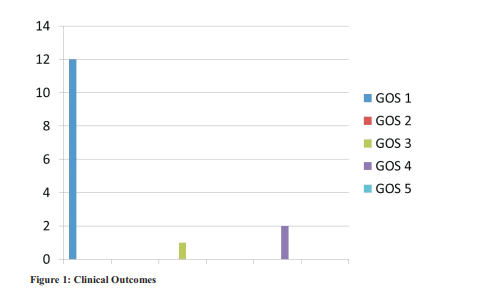
Results: Sixteen patients had neurosurgical procedures for SICH but only 15 had
complete data. Males were 13/15(86.7%) and most (66.7%) had admission GCS =8.
The mean age was 58.8years (range: 34-80). Most of the patients were elderly
(53.3%). Systemic hypertension was the cause in 14(93.3%). There was right-sided
and lobar predominance (60.0% and 46.7% respectively) and most (80.0%) had
intraventricular extension. The commonest procedure was external ventricular
drainage (86.7%) with or without craniotomy (20.0%) / burr hole (13.3%) for
haematoma evacuation. Twelve (80.0%) of the patients died. Predictors of poor
outcome were low admission GCS, brainstem dysfunction, aspiration/chest
infection, seizures and long ictus-to-operation time. Identified challenges of care
included delay in presentation, delay in getting CT, difficulty with blood pressure
control, lack of hospital facilities and tortuous referral pathway.
Conclusion: The high mortality of SICH and its gloomy outlook may be
improved upon by tackling the various identified challenges surrounding its
care.
References
Murray CJ, Lopez AD. Mortality by cause for
eight regions of the world: Global Burden of
Disease Study. Lancet. 1997; 349:1269-76
Sacco RL. Risk factors, outcomes, and stroke
subtypes for ischemic stroke. Neurology. 1997;
(5 Suppl 4):S39-44
Javed G, Tahir MZ, Enam SA. Role of
neurosurgery in the management of stroke. J Pak
Med Assoc. 2008; 58(7):378-384
Goldstein LB, Simel DL. Is this patient having a
stroke? JAMA. 2005; 293:2391-402
Zhang X-q, Zhang Z-m, Yin X-l, Zhang K, Cai H,
Ling F. Exploring the optimal operation time for
patients with hypertensive intracerebral
hemorrhage: tracking the expression and
progress of cell apoptosis of prehematomal brain
tissues. Chinese Medical Journal. 2010; 123(10).
PMID: 20529574
Raafat M, Ragab OA, Abdelwahab OM, Salama
MM, Hafez MA. Early versus delayed surgical
evacuation of spontaneous supratentorial
intracerebral hematoma: A prospective cohort
study. Surg Neurol Int. 2020; 11:145.
https://doi.org/10.25259/SNI_103_2020 PMID:
Schirmer CM, Hoit DA, Malek AM.
Decompressive hemicraniectomy for the
treatment of intractable intracranial hypertension
after aneurysmal subarachnoid hemorrhage.
S t r o k e . 2 0 0 7 ;
(3):987–92.https://doi.org/10.1161/01.STR.0
58269.e2 PMID: 17272765
Kim KH, Ro YS, Park JH, Jeong J, Shin SD,
Moon S. Association between time to emergency
neurosurgery and clinical outcomes for
spontaneous hemorrhagic stroke: A nationwide
observational study. PLoS ONE. 2022; 17(4):
e 0 2 6 7 8 5 6 .
https://doi.org/10.1371/journal.pone.0267856
Connor MD, Walker R, Modi G, Warlow CP.
Burden of stroke in black populations in subSaharan Africa. Lancet Neurol. 2007; 6:269–78.
doi:10.1016/S1474- 4422(07)70002-9
Feigin VL, Lawes CM, Bennett DA, BarkerCollo SL, Parag V. Worldwide stroke incidence
and early case fatality reported in 56 populationbased studies: a systematic review. Lancet
Neurol. 2009; 8:355–69. doi:10.1016/S1474-
(09)70025-0
O'Donnell MJ, Xavier D, Liu L, Zhang H, Chin
SL, Rao-Melacini P, et al. Risk factors for
ischaemic and intracerebral haemorrhagic stroke
in 22 countries (the INTERSTROKE study): a
case-control study. Lancet. 2010; 376:112–23.
doi:10.1016/S0140-6736(10)60834-37
Owolabi MO. Taming the burgeoning stroke
epidemic in Africa: stroke quadrangle to the
rescue. West Indian Med J. 2011; 60:412–21
Adeleye AO, Osazuwa UA and Ogbole GI. The
clinical epidemiology of spontaneous ICH in a
sub-Sahara African country in the CT scan era: a
neurosurgical in-hospital cross-sectional survey.
Fr o n t. N e u r o l. 2 0 1 5 ; 6 : 1 6 9 . d o i:
3389/fneur.2015.00169
Sagui E. Stroke in Sub-Saharan Africa. Med Trop
(Mars). 2007; 67:596-600
van Asch CJ, Luitse MJ, Rinkel GJ, van der
Tweel I, Algra A, Klijn CJ. Incidence, case
fatality, and functional outcome of intracerebral
haemorrhage over time, according to age, sex,
and ethnic origin: A systematic review and
meta-analysis. Lancet Neurol. 2010; 9:167-76
Ndubuisi CA, Okhueleigbe MO, Mbadugha TN,
Ndukuba KO, Inojie MO, Ohaegbulam SC.
Factors influencing the outcome of spontaneous
intracerebral haematoma in a Neurosurgical
Hospital in South-East Nigeria. Niger Postgrad
M e d J. 2 0 1 9 ; 2 6 ( 2 ): 11 3 - 11 7 . d o i:
4103/npmj.npmj_22_19
Jenkins C, Ovbiagele B, Arulogun O, Singh A,
Calys-Tagoe B, Akinyemi R, et al. Knowledge,
attitudes and practices related to stroke in Ghana
and Nigeria: A SIREN call to action. PLoS ONE.
; 13(11): e0206548
Owolabi MO, Akarolo-Anthony S, Akinyemi R,
Arnett D, Gebregziabher M, Jenkins C, et al. The
burden of stroke in Africa: a glance at the present
and a glimpse into the future. Cardiovasc J Afr.
; 26(2Suppl. 1): S27–S38
Lozano R, Naghavi M, Foreman K, Lim S,
Shibuya K, Aboyans V, et al. Global and regional
mortality from 235 causes of death for 20 age
groups in 1990 and 2010: a systematic analysis
for the Global Burden of Disease Study 2010.
Lancet. 2012; 380(9859): 2095–2128
Komolafe MA, Ogunlade O, Komolafe EO.
Stroke mortality in a teaching hospital in South
Western Nigeria. Trop Doct. 2007; 37:186-8
Ogun SA. Acute stroke mortality at LUTH. Niger
J Clin Pract. 2003; 5:38-41
Wahab KW, Okubadejo NU, Ojini FI, Danesi
MA. Predictors of short-term intra-hospital case
fatality following first-ever acute ischaemic
stroke in Nigerians. J Coll Physicians Surg Pak.
; 18:755-8
Tobi K, Okojie N. Characteristics and outcome of
stroke patients with cerebrovascular accident at
the intensive care unit of a tertiary hospital in
Nigeria. J West Afr Coll Surg. 2013; 3(1):1-13.
PMID: 25453008; PMCID: PMC4228813
Aiwansoba IF, Chukwuyem OW. Early postacute stroke seizures: clinical profile and
outcome in a Nigerian stroke unit. Ann Afr Med.
; 13(1):11–15
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Research Journal of Health Sciences

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Research Journal of Health Sciences journal is a peer reviewed, Open Access journal. The Journal subscribed to terms and conditions of Open Access publication. Articles are distributed under the terms of Creative Commons License (CC BY-NC-ND 4.0). (http://creativecommons.org/licences/by-nc-nd/4.0). All articles are made freely accessible for everyone to read, download, copy and distribute as long as appropriate credit is given and the new creations are licensed under the identical terms.

