Hypoxaemia and its clinical predictors among children with pneumonia at a tertiary centre in Osogbo, Southwestern, Nigeria.
Keywords:
Hypoxaemia, pneumonia, hospitalized children, under-fives, clinical predictorsAbstract
Objective: Hypoxaemia is a feature of severe pneumonia particularly among children aged less than five years. This study aimed to determine the prevalence and clinical predictors of hypoxaemia among children with pneumonia.
Methods: It was a hospital-based cross-sectional observational study involving 129 children aged 1 - 59 months with both clinical and radiological pneumonia. The haemoglobin oxygen saturation (SPO2) was obtained at presentation. Hypoxaemia was defined as SPO2 < 90 percent.
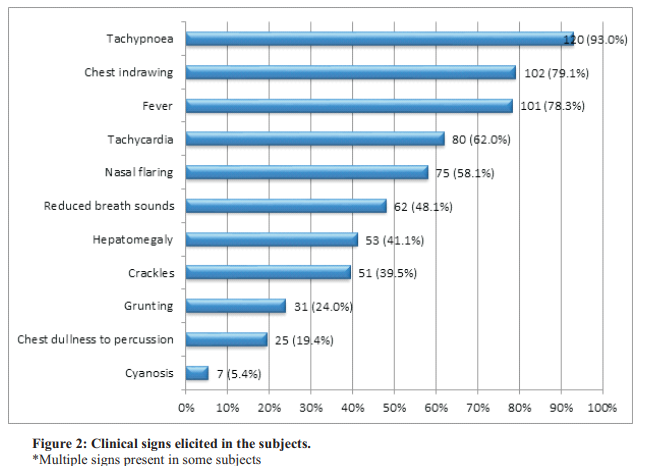
Result: Of the129 subjects studied, 49 (38.0%) had hypoxaemia. The clinical signs that were significantly associated with hypoxaemia were central cyanosis (p= 0.012), grunting (p= 0.014), nasal flaring (p< 0.001), lethargy (p< 0.001), restlessness (p= 0.002), loss of consciousness (p< 0.001), and inability to feed (p< 0.001). A combination of nasal flaring with central cyanosis, grunting or tachypnoea were significant predictors of hypoxaemia (p= 0.029, 0.017 and <0.001 respectively). Tachypnoea and nasal flaring had the highest sensitivity and specificity among the clinical signs for hypoxaemia. Prolonged hospital stay (> 5 days) and mortality were significantly associated with hypoxaemia (p< 0.001).
Conclusion: Hypoxaemia is common among children hospitalized for pneumonia. It is an important determinant of hospital stay and outcome.
References
Aderele WI and Johnson WBR. Pneumonias. In:
Azubuike JC, Nkanginieme KE. (eds.)
Paediatrics and child health in a tropical region.
nd edition. Owerri, Nigeria: University of PortHarcourt press; 2007 p. 425- 427.
World Health Organisation. Pneumonia Fact s h e e t . A v a i l a b l e f r o m :
http://www.who.int/mediacentre/factsheets/fs33 1/en/. [Assessed 4th April 2020].
Rudan I, Boschi-pinto C, Biloglav Z, Mulholland K, Campbell H. Epidemiology and etiology of childhood pneumonia. Bull WHO 2008; 86: 408 - 416.
Walker CLF, Rudan I, Liu I, Nair H, Theodoratou E, Bhutta ZA, et al. 'Global burden of childhood pneumonia and diarrhoea', Lancet 2013;381( 9875): 1405–1416.
UNICEF. Nigeria contributes highest number to global pneumonia child deaths. Available from: https://www.unicef.org/. [Accessed 1st May 2020].
World Health Organisation. Oxygen therapy for children. Geneva: WHO; 2016. Available from: http://apps.who.int/iris/bitstream/10665/204584 /1/9789241549554_eng.pdf. [Accessed 4th May 2020].
Lozano JM. Epidemiology of hypoxaemia in children with acute lower respiratory infection. Int J Tuberc Lung Dis 2001; 5 (6): 496 – 504.
Abdulkadir MB, Ibraheem RM, Gobir AA, Johnson WBR. Hypoxaemia as a measure of disease severity in young hospitalized Nigerian children with pneumonia: A cross-sectional study. S Afr J Ch 2015; 9 (2): 53 - 56.
Usen S and Weber M. Clinical signs of hypoxaemia in children with acute lower respiratory infection: indicators of oxygen therapy. Int J Tuberc Lung Dis 2001; 5 (6): 505 - 510.
Sarkar M, Niranjan N, Banyal Sarkar M, Niranjan N, Banyal PK. Mechanisms of hypoxaemia.
Lung India 2017; 34 (1): 47 - 60.
Kuti BP, Adegoke SA, Oyelami OA, Ota MO. Predictors of prolonged hospitalisation in childhood pneumonia in a rural health centre. S Afr J Ch 2014; 8 (1): 11 - 15.
Usen S, Weber M, Mulholland K, Jaffer S,
Oparuago A, Adegbola R et al. Clinical predictors of hypoxaemia in Gambian children with acute lower respiratory tract infection: prospective cohort study. BMJ 1999; 318: 86 - 91.
Lee WW, Mayberry K, Crapo R, Jensen RL. The accuracy of pulse oximetry in the emergency department. Am J Emerg Med 2000;18(4): 427- 431.
World Health Organization. Revised WHO classification and treatment of childhood pneumonia at health facilities - Evidence
S u m m a r i e s . A v a i l a b l e f r o m :
http://www.who.int/maternal_child_adolescent/ documents/child-pneumonia-treatment/en/. [Accessed 30th April 2020]
Araoye MA. Subject Selection in Research
Methodology with statistics for Health and Social Sciences. Ilorin, Nigeria: Nathadex Publishers; 2004 p. 115 - 129.
Emodi IJ, Ikefuna AN, Ubesie AC, Chukwu BF, Chinawa JM. Assesment of clinical features and haematocrit levels in detection of hypoxaemia in sick children. Afr J Resp Med 2011; 7 (1): 11 – 13.
Swatch M. Doctor and Patient. In: Swatch M (ed.) Hutchinson's Clinical Methods. 20th edition. London: WB Saunders; 1995 p. 1 - 22.
Molyneux ME, Taylor TE, Wirima JJ, Borgstein A. Clinical features and prognostic indicators in paediatric cerebral malaria: a study of 131 comatose Malawian children. Q J Med1989; 71: 441– 59.
Cherian T, Mulholland EK, Carlin JB, Ostensen H, Amin R, Campo M, et al. Standardized interpretation of paediatric chest radiographs for the diagnosis of pneumonia in epidemiological studies. Bull WHO 2005; 83 (5): 353 – 359.
Lozano JM. Epidemiology of hypoxaemia in children with acute lower respiratory infection. Int J Tuberc Lung Dis 2001; 5 (6): 496 – 504.
Basnet S, Adhikari RK, and Gurung CK. Hypoxaemia in Children with Pneumonia and Its Clinical Predictors. Indian J Pediatr 2006; 73 (9): 777 - 781.
Motwani NP, Janakiraman L, Bala SS, and Bhawnani D. Clinical Predictors of Hypoxaemia in Children with Acute Lower Respiratory
Illness. Int Res J Med Sci 2015; 3 (3): 11 - 15.
Graham H, Bakare AA, Ayede AI, Oyewole OB, Gray A, Peel D et al. Hypoxaemia in hospitalised children and neonates: A prospective cohort study in Nigerian secondary-level hospitals.
EClinicalMedicine 2019;16: 51- 63.
Qureshi SA. Measurement of respiratory function: an update on gas exchange. Anaesth Intens Care Med 2011; 12: 490 - 495.
Onyango FE, Steinhoff MC, Wafula EM, Musia J, Wariua S, Musia J et al. Hypoxaemia in young Kenyan children with acute lower respiratory infection. BMJ 1993; 306: 612 - 615.
Heing NR, Pierson DJ. Mechanism of hypoxaemia. Resp Care Clin N Am 2000; 6: 501 - 521.
Grocott M, Montgomery H, and Vercueil A. Highaltitude physiology and pathophysiology: implications and relevance for intensive care medicine. Crit Care 2007; 11 (1): 203.
Rodriguez-Roisin R and Roca J. Update '96 on pulmonary gas exchange pathophysiology in pneumonia. Seminars in Respiratory Infections 1996;11 (1):3-12.
Sah HD. Study of predictors of hypoxaemia in children with Pneumonia. J Coll Med Sci Nepal 2013; 9 (4): 1 - 8.
Tiewsoh K, Lodha R, Pandey RM, Broor S, Kalaivani M, and Kabra SK. Factors determining the outcome of children hospitalized with severe pneumonia. BMC Pediatr 2009; 9:15.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Research Journal of Health Sciences

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Research Journal of Health Sciences journal is a peer reviewed, Open Access journal. The Journal subscribed to terms and conditions of Open Access publication. Articles are distributed under the terms of Creative Commons License (CC BY-NC-ND 4.0). (http://creativecommons.org/licences/by-nc-nd/4.0). All articles are made freely accessible for everyone to read, download, copy and distribute as long as appropriate credit is given and the new creations are licensed under the identical terms.

