Sleep quality and psychological morbidity among physicians in southwest Nigeria
Keywords:
Sleep quality, psychological morbidity, physicians, work schedules, NigeriaAbstract
Objectives: The role of the physician has increasingly become more expansive, and demanding. These demanding schedules have played a heavy toll on sleep patterns and increased psychological stress. The objective of the study was to assess sleep quality and psychological morbidity among Physicians.
Method: A cross-sectional survey of 95 voluntary consenting physicians from different specialties during a 2-day conference. We administered Pittsburgh Sleep Quality Index, and General Health Questionnaire12.
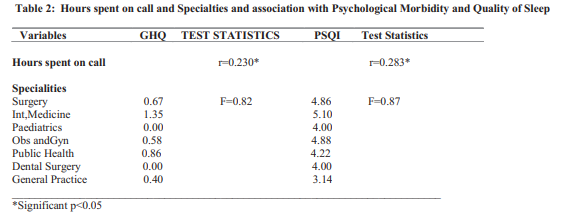
Results; About 13.6% (n=13 out of 95) had a score above 2 on General Health Questionnaire-12, indicating psychological morbidity. Those who reported poor sleep quality (>5) made up 36.8% (n=35) of the respondents, There were positive significant correlation between hours spent on call and total scores on GHQ at r=0.230, p=0.03. Only subjective sleep quality (component 1) was significantly correlated with total GHQ scores at p=0.001
Conclusion: The findings in our study showed a relationship between sleep quality (component 1) psychological morbidity. We observed that long work schedules was the only factor associated with psychological morbidity and sleep quality. It is imperative for work-time stress management to be instituted among physicians.
References
Shakespeare W, Sanders N. Othello (The New Cambridge Shakespeare).1984
Min AA, Sbarra DA, Keim SM. Sleep disturbances predict prospective declines in resident physicians' psychological well-being. Medical education online. 2015 Jan 1; 20(1):28530.
Papp KK, Stoller EP, Sage P, Aikens JE, Owens J, Avidan A, et al. The effects of sleep loss and fatigue on resident-physicians: A multiinstitutional, mixed-method study. Acad Med. 2004;79:394–406.
Vela-Bueno A, Moreno-Jiménez B, RodríguezMuñoz A, Olavarrieta-Bernardino S, FernándezMendoza J, De la Cruz-Troca JJ, et al. Insomnia and sleep quality among primary care physicians with low and high burnout levels. J Psychosom Res. 2008; 64: 435–42.
Landrigan CP, Rothschild JM, Cronin JW,
Kaushal R, Burdick E, Katz JT, et al. Effect of reducing interns' work hours on serious medical errors in intensive care units. N Engl J Med. 2004;351:1838–48.
Aliyu I, Mohammed II, Lawal TO, Gudaji M, Garba N, Monsudi KF, Michael GC, Peter ID. Assessment of sleep quality among medical doctors in a Tertiary Hospital in a semi-rural setting. Journal of neurosciences in rural practice. 2018 Oct; 9(4):535.
Buysse, Daniel J.; Reynolds, Charles F.; Monk, Timothy H.; Berman, Susan R.; Kupfer, David J. (May 1989). "The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research". Psychiatry Research. 28 (2): 193–213. doi:10.1016/0165-1781(89)90047-4. PMID 2748771.
Aloba OO, Adewuya AO, Ola BA, Mapayi BM. Validity of the Pittsburgh sleep quality index
(PSQI) among Nigerian university students Sleep medicine; 2015; 8(3), 266-70
Qin M, Vlachantoni A, Evandrou M, Falkingham J. General Health Questionnaire-12 reliability, factor structure, and external validity among older adults in India. Indian journal of psychiatry. 2018 Jan;60(1):56
Dowell AC, Hamilton S, McLeod DK. Job satisfaction, psychological morbidity and job stress among New Zealand general practitioners. New Zealand Medical Journal. 2000 Jul 14; 113(1113):269.
Issa BA, Yussuf AD, Olanrewaju GT, Abiodun OA. Mental health of doctors in a tertiary hospital in Nigeria. The Pan African medical journal. 2014; 19.
Ogualili PN, Anyiam DC, Ezejiofor OI. Prevalence of Psychiatric Morbidity among Medical Practitioners in an Urban Town in Nigeria. Orient Journal of Medicine. 2017; 29(34):98-105.
Abiodun OA. A study of mental morbidity among primary care patients in Nigeria. Comprehensive psychiatry. 1993 Jan 1; 34(1):10-3.
Markwell AL, Wainer Z. The health and wellbeing of junior doctors: insights from a national survey. Medical Journal of Australia. 2009 Oct; 191(8):441-4.
Kolo ES, Ahmed AO, Hamisu A, Ajiya A,
Akhiwu BI. Sleep health of healthcare workers in Kano, Nigeria. Nigerian journal of clinical practice. 2017;20(4):479-83
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Research Journal of Health Sciences

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Research Journal of Health Sciences journal is a peer reviewed, Open Access journal. The Journal subscribed to terms and conditions of Open Access publication. Articles are distributed under the terms of Creative Commons License (CC BY-NC-ND 4.0). (http://creativecommons.org/licences/by-nc-nd/4.0). All articles are made freely accessible for everyone to read, download, copy and distribute as long as appropriate credit is given and the new creations are licensed under the identical terms.

