Assessment of challenges inhibiting effective delivery of health care services among frontline Professional health workers during COVID-19 Lock down in Nigeria
DOI:
https://doi.org/10.4314/rejhs.v11i1.4Keywords:
COVID 19, health care delivery, frontline workers, social distancing, telemedicineAbstract
Background: Coronavirus (COVID-19) increased patient loads globally, having a negative impact on health services. Social distancing is one strategy to prevent spreading COVID-19 but creates challenges for health professionals. This study assessed the challenges of COVID-19 for selected health professionals in Nigeria.
Methodology: This is a cross-sectional survey of challenges inhibiting health care service provision during COVID 19 lockdown. Data collected with a pretested online self-administered questionnaire
included age, gender, occupation, place of practice, physical distance practices, utilization of telemedicine, income and other concerns that may have inhibited their practices during the COVID 19 lockdown. Data were analyzed using a statistical package for social sciences (SPSS) version 26.0 with the level of significance set at p<0.05. Chi square goodness of fit test was used to analyze the association between means and qualitative variables.
Results: Response rate from 599 questionnaires was 481 (78%) with physiotherapists (n=108, 23%);
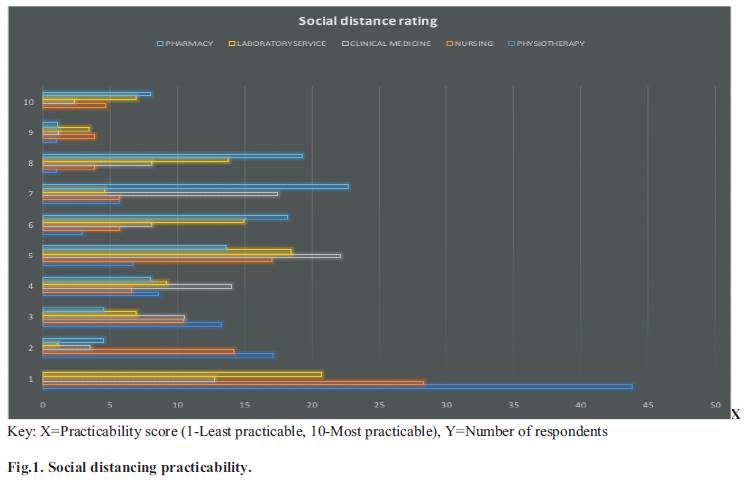
nurses (n=106, 22%); doctors (n=86, 18%); laboratory technicians (n=87, 18%) and pharmacists (n=94,19%); in public sector (n=318, 66%) and private practitioners (n=163, 34%). During the “lockdown” patients interacting with health professionals in private practice decreased except increases for laboratory technicians (11.91%) and pharmacists (68.35%). Social distancing was feasible by pharmacists and laboratory technicians, but interactions by nurses, physiotherapists and doctors were compromised. Telemedicine was used mostly by doctors (n=42, 48.8%), and physiotherapists (n=50, 46.3%). Health professionals experienced mental stress 428 (89%); anxiety 176 (37%); feared infection 333 (69%) and 232 (48%) of transmitting to their families; 307 (64 %) had challenges with personal protective equipment. Suggestions were: alternate accommodation or longer shifts with less working days 111(37%); a hazard allowance 244(51%) and counseling 238(49%).
Conclusion: Private practitioners reported a loss of income with all health professionals indicating the "lockdown" and COVID-19 compromised health delivery, health services, and individuals' health. Health professionals suggested a hazard allowance, alternate accommodation, and dedicated counseling for health professionals during the pandemic.
References
WHO. Wo r l d He a l t h Or g a n i s a t i o n . [https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-research-on-novelcoronavirus-2019-ncov]. 2019 [novel coronavirus Accessed on 12th of April, 2020.].
WHO. World Health Organisation COVID 19 [https://covid19.who.int]. 2020 [COVID-19 Pandemics. Accessed on 2nd of April, 2020].
Shanafelt T, Ripp J, Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. Jama. 2020;323(21):2133-4.
Wiederhold BK, Cipresso P, Pizzioli D, Wiederhold M, Riva G. Intervention for Physician Burnout: A Systematic Review. Open Med (Wars). 2018;13(1):253-63.
Fred HL, Scheid MS. Physician Burnout: Causes, Consequences, and (?) Cures. Tex Heart Inst J. 2018;45(4):198-202.
Liebenberg AR, Coetzee JFJ, Conradie HH, Coetzee JF. Burnout among rural hospital doctors in the Western Cape: Comparison with previous South African studies. African journal of primary health care & family medicine. 2018;10(1):1-7.
Kannampallil TG, Goss CW, Evanoff BA, Strickland JR, McAlister RP, Duncan J. Exposure to COVID-19 patients increases physician trainee s t r e s s a n d b u r n o u t . P L o S O n e . 2020;15(8):e0237301.
Singhal T. A Review of Coronavirus Disease-2019 (COVID-19). Indian J Pediatr. 2020;87(4):281-6.
Zhang L, Liu Y. Potential interventions for novel coronavirus in China: A systematic review. J Med Virol. 2020;92(5):479-90.
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020;382(8):727-33.
Adepoju P. Nigeria responds to COVID-19; first case detected in sub-Saharan Africa. Nature medicine. 2020;26(4):444.
Haider N, Yavlinsky A, Simons D, Osman AY, Ntoumi F, Zumla A, et al. Passengers' destinations from China: low risk of novel coronavirus (2019-nCoV) transmission into Africa and South America. Epidemiology & Infection. 2020;148.
Nkengasong JN, Mankoula W. Looming threat of COVID-19 infection in Africa: act collectively, and fast. Lancet. 2020;395(10227):841-2.
Gilbert M, Pullano G, Pinotti F, Valdano E, Poletto C, Boelle PY, et al. Preparedness and vulnerability of African countries against importations of COVID-19: a modelling study. Lancet. 2020;395(10227):871-7.
Wong MC, Huang J, Teoh JY, Wong SH. Identifying capability framework that could mitigate the COVID-19 pandemic in global health community. The Journal of infectious diseases. 2020.
Ren LL, Wang YM, Wu ZQ, Xiang ZC, Guo L, Xu T, et al. Identification of a novel coronavirus causing severe pneumonia in human: a descriptive study. Chin Med J (Engl). 2020;133(9):1015-24.
Soriano V, Barreiro P. Impact of New Coronavirus Epidemics on HIV-Infected Patients. AIDS Rev. 2020;22(1):57-8.
Zhu F, Cao Y, Xu S, Zhou M. Co-infection of SARS-CoV-2 and HIV in a patient in Wuhan city, China. Journal of Medical Virology. 2020.
Grobler L, Mehtar S, Dheda K, Adams S, Babatunde S, van der Walt M, et al. The epidemiology of tuberculosis in health care workers in South Africa: a systematic review. BMC Health Serv Res. 2016;16(1):416.
FMOH. Health Minister: First Case Of Covid-19 Confirmed In Nigeria. 2020.
NCDC. Case Summary In Nigeria as at April 16th 2020. 2020.
Mazanec P. COVID-19 Resource: Ethical dilemmas facing nurses during the Coronavirus Crisis: Addressing moral distress.
Etkind SN, Bone AE, Lovell N, Cripps RL, Harding R, Higginson IJ, et al. The Role and Response of Palliative Care and Hospice Services in Epidemics and Pandemics: A Rapid Review to Inform Practice During the COVID-19 Pandemic. J Pain Symptom Manage. 2020;60(1):e31-e40.
Onyemelukwe I, Nwankwo O. A REVIEW OF THE REGULATORY FRAMEWORK FOR MATERNAL HEALTH IN NIGERIA.
Statista. Population of Nigeria in selected years between 1950 and 2020. 2020.
System CR. The Survey system. 2012.
Huijbregts MP, Myers AM, Kay TM, Gavin TS. Feature articles-systematic outcome measurement in clinical practice: challenges experienced by physiotherapists. Physiotherapy Canada. 2002;54(1):25-31.
Dillman DA SJ, Christian LM. . Internet, mail, and mixed-mode surveys:. The tailored design method. 2008;vol. 3rd ed. 2008.
Bootsma M, Ferguson N. The effect of public health measures on the 1918 influenza pandemic in US cities. Proc Natl Acad Sci. 2007.
Bootsma MCJ FN. The effect of public health measures on the 1918 influenza pandemic in US cities. Proc Natl Acad Sci. 2007.
Markel H LH, Navarro JA, Sloan A, Michalsen JR, Stern AM, et al. Nonpharma- ceutical interventions implemented by US cities during the 1918-1919 influenza pandemic.. JAMA. 2007:298(6):644–54.
Hatchett RJ, Mecher CE, Lipsitch M. Public health interventions and epidemic intensity during the 1918 influenza pandemic. Proc Natl Acad Sci U S A. 2007;104(18):7582-7.
Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med. 2020;27(2):27(2).
Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD. How will country-based mitigation measures influence the course of the COVID- 1 9 e p i d emi c ? T h e L a n c e t . 2020;395(10228):931-4.
Cohen J, Kupferschmidt K. Countries test tactics in 'war'against COVID-19. American Association for the Advancement of Science; 2020.
Koren M, Peto R. Business disruptions from social distancing. PLoS One. 2020;15(9):e0239113.
Alami H, Gagnon MP, Fortin JP. Some Multidimensional Unintended Consequences of Telehealth Utilization: A Multi-Project Evaluation Synthesis. Int J Health Policy. 2019;8(6):337-52.
Theodoros D, Hill A, Hartley N, Martin-Khan M, Bird D, Russell T, et al. Innovation to implementation for telehealth (i2i4Telehealth). A practical guide for knowledge translation in telehealth. 2016.
AlDossary S, Martin-Khan MG, Bradford NK, Armfield NR, Smith AC. The Development of a Telemedicine Planning Framework Based on Needs Assessment. Journal of Medical Systems. 2017;41(5):74.
Downar J aSD. Palliating a pandemic: all patients must be cared for. J Pain Symptom Manage. 2010;39.
Catton H. Global challenges in health and health care for nurses and midwives everywhere. Int Nurs Rev. 2020;67(1):4-6.
Huang J, Han M, Luo T, Ren A, Zhou X. Mental health survey of 230 medical staff in a tertiary infectious disease hospital for COVID-19. Zhonghua lao dong wei sheng zhi ye bing za zhi=Zhonghua laodong weisheng zhiyebing zazhi=Chinese journal of industrial hygiene and occupational diseases. 2020;38:E001-E.
Mahraj S, Ranjiah P. The prevalence of comorbidities in patients on HAART referred for physiotherapy in three public hospitals in KwaZulu-Natal, South Africa: a short report. South African Journal of Physiotherapy. 2010;66(3):21-4.
Schuklenk U. What healthcare professionals owe us: why their duty to treat during a pandemic is contingent on personal protective equipment (PPE). Journal of medical ethics. 2020.
Rose C. Am I part of the cure or am I part of the disease? Keeping coronavirus out when a doctor comes home. New England Journal of Medicine. 2020;382(18):1684-5.
Rodriguez-Morales AJ, Cardona-Ospina JA, Gutierrez-Ocampo E, Villamizar-Pena R,Holguin-Rivera Y, Escalera-Antezana JP, et al. Clinical, laboratory and imaging features of COVID-19: A systematic review and metaanalysis. Travel Med Infect Dis. 2020;34:101623.
Kang L, Li Y, Hu S, Chen M, Yang C, Yang BX, etal. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. 2020;7(3):e14.
Odebiyi OD AB. Gender distribution of Physiotherapy graduates from Nigerian Universities. J Niger Soc Physiother. 2005:15:45–7.
Emeribe V, Akah L. Knowledge, Attitude and Participation of Male and Female Nurses in Recreational Activities in Cross River State, Nigeria. Canadian Social Science. 2012;8(4):150-3.
Chersich MF, Gray G, Fairlie L, Eichbaum Q, Mayhew S, Allwood B, et al. COVID-19 in Africa: care and protection for frontline healthcare workers. Globalization and Health. 2020;16:1-6.
Hu Z, Song C, Xu C, Jin G, Chen Y, Xu X, et al. Clinical characteristics of 24 asymptomatic infections with COVID-19 screened among close contacts in Nanjing, China. Science China Life Sciences. 2020;63(5):706-11
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Research Journal of Health Sciences

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Research Journal of Health Sciences journal is a peer reviewed, Open Access journal. The Journal subscribed to terms and conditions of Open Access publication. Articles are distributed under the terms of Creative Commons License (CC BY-NC-ND 4.0). (http://creativecommons.org/licences/by-nc-nd/4.0). All articles are made freely accessible for everyone to read, download, copy and distribute as long as appropriate credit is given and the new creations are licensed under the identical terms.





