The factors influencing uptake of Provider Initiated Testing and counselling of HIV in a rural primary health care centre in the Eastern Cape.
Keywords:
Opt-out HIV testing, pregnant women, stigma, VCTAbstract
Background: Access to HIV care begins with the process of undergoing HIV testing. Factors that affect the knowledge, attitude and practices of antenatal attendees towards routine HIV testing could affect its uptake.
Objectives: This study was to determine the factors influencing uptake of routine HIV testing amongst antenatal attendees at Baziya Health Centre, Eastern Cape, South Africa.
Materials & Methods: This was a descriptive study where 96 respondents were interviewed from November 2010 to January 2011. Participants were selected consecutively. A pre-tested, pre-coded, closed interview schedule was used. There were 96 participants in the study.
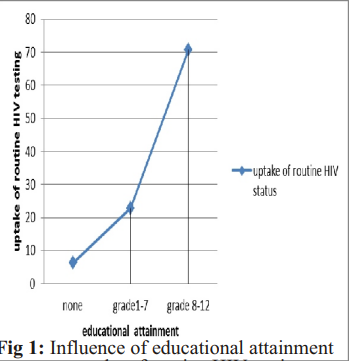
Results: The mean age of the subjects was 23.8 years ± 15, median of 22 years and a mode of 18 years.The range was 16 - 38 years. The following variables respectively were found as facilitating factors to routine HIV testing patterns: increase in education attainment (AOR 22.7 (1.4-100), p=0.039), influence of group counselling (AOR21 (6-91.5), p=0.005), health worker involvement (AOR 11.9 (271.4), p=0.046). Stigma was found to be a constraining factor to routine HIV testing (AOR27.7 (5-150.3), p=0.0001).
Conclusion: The uptake of routine HIV testing amongst pregnant women in Baziya was facilitated by the level of educational attainment, group counselling, and health care workers involvement. Stigma was found to prevent uptake of routine HIV testing. The intervention strategies to maximise routine HIV testing acceptance should focus on education level, group counselling, psychological status and social support. Measures should be implemented to protect against HIV associated stigma.
References
Ghys P, Walker N, Mcfarland W, Miller R,Garnett G. Improved data, methods and tools for the 2007 HIV and AIDS estimates and projections. Sexually Transmitted Infections, 2008; 84: 1.
Department of Health. National Antenatal Sentinel HIV and Syphilis Prevalence Survey in South Africa, 2010; 1: 50.
Magongo B, Magwaza S, Mathambo V, Makhanya N. National report on the assessment of the public sector's voluntary counseling and testing programme. Health Systems Trust. Durban, South Africa. 2002; 1-20.
Bayer R. &Edington C. HIV testing, human rights, and global AIDS policy: exceptionalism and its discontents. Journal of health politics, policy and law, 2009; 34: 301-323.
Branson BM, Handsfield H H, Lampe M A, Janssen RS, Taylor AW, Lyss SB. et al. National Center for HIV/AIDS & Prevention. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings, US Department of Health and Human Services, Centers for Disease Control and Prevention. 2006; 55: 1-17.
Bassett IV, Walensky RP. Integrating HIV screening into routine health care in resource-limited settings. Clinical Infectious Diseases. 2010; 50: 77-84.
Peltzer K, Matseke G, Mzolo T, Majaja M. Determinants of knowledge of HIV status in South Africa: results from a population-based HIV survey. BMC public health, 2009; 9: 174.
Hendriksen E S, Hlubinka D,
Chariyalertsak S, Chingono A, Gray G, Mbwambo J. et al. Keep talking about it: HIV/AIDS-related communication and prior HIV testing in Tanzania, Zimbabwe, South Africa, and Thailand.
AIDS and Behavior. 2009; 13: 12131221.
Omoera OS, Awosola KR, Okhakhu, MA.Adesina AA. HIV/AIDS and the Broadcast Media in Urban Communities in Edo State, Nigeria. International Journal. 2010; 4: 1-13.
Koker P, Lefèvre P, Matthys F, Stuyft P, Delva W. Barriers to VCT despite 13 years of community-based awareness campaigns in a peri-urban township in
Northern Limpopo. South African Medical Journal. 2010; 100: 364-365.
Iliyasu Z, Abubakar I, Kabir M, Aliyu
M. Knowledge of HIV/AIDS and attitude towards voluntary counseling and testing among adults. Journal of the National Medical Association. 2006; 98:1917-1922.
Wanyenze R, Nawavvu C, Namale A, Mayanja B, Bunnell R, Abang B. Et al.
Acceptability of routine HIV counselling and testing, and HIV seroprevalence in Ugandan hospitals. Bulletin of the World Health
Organization. 2008; 86: 302-309.
Weiser SD, Heisler M, Leiter K, PercyDe Korte F, Tlou S. Demonner S. et al. Routine HIV testing in Botswana: a population-based study on attitudes, practices, and human rights concerns. PLoS medicine. 2006; 3: 261.
Abiodun M, Munir'deen A, Aboyeji P. Awareness and knowledge of mother-tochild transmission of HIV among pregnant women. Journal of the National Medical Association. 2007; 99: 758.
Nguyen H, Gammeltoft T, Rasch V. Early uptake of HIV counseling and testing among pregnant women at different levels of health facilities - experiences from a community-based study in Northern Vietnam. BMC Health Services Research. 2011; 11: 29.
Hutchinson P, Mahlalela X.
Utilization of voluntary counseling and testing services in the Eastern Cape, South Africa. AIDS care, 2006; 18: 446455.
Bokhour B, Solomon J, Knapp H, Asch S, Gifford A . Barriers and facilitators to routine HIV testing in VA primary care. Journal of general internal medicine. 2009; 24: 1109-1114.
Asante A D. Scaling up HIV prevention: why routine or mandatory testing is not feasible for sub-Saharan Africa. Bulletin of the World Health Organization. 2007; 85: 644-646.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Research Journal of Health Sciences

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Research Journal of Health Sciences journal is a peer reviewed, Open Access journal. The Journal subscribed to terms and conditions of Open Access publication. Articles are distributed under the terms of Creative Commons License (CC BY-NC-ND 4.0). (http://creativecommons.org/licences/by-nc-nd/4.0). All articles are made freely accessible for everyone to read, download, copy and distribute as long as appropriate credit is given and the new creations are licensed under the identical terms.

