Prevalence of Gram-negative bacteria and their antibioticresistance pattern at tertiary care hospital Amreli Gujarat India
DOI:
https://doi.org/10.4314/rejhs.v11i1.2Keywords:
Gram-negative bacteria, clinical samples, antibiotic resistant pattern, multi-drug resistantAbstract
Background: Infections with multi-drug resistant (MDR) bacteria are serious threats to healthcare services many low-income countries associated with overuse and misuse of antibiotics.
Material and Methods: A prospective cross-sectional study was done between January, 2021 to December, 2021 at Shantabaa Medical College and General Hospital, Amreli, Gujarat, India. Clinical specimens such as swab from wound, urine, sputum, blood, body fluids and throat swab were sampled following standard operating procedures.
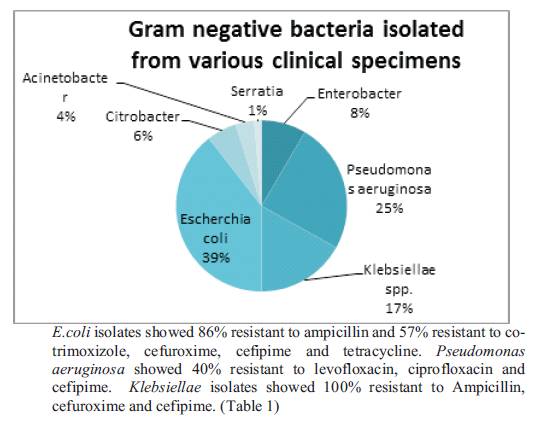
Results: A total of 738 patient specimens were collected and processed from different clinical samples such as urine 540 (73%), wound swab 48 (6.5%), sputum 96 (13%), blood 06 (1%), throat swab 12(1.5%)and other body fluids 36 (5%). Overall, 142 (19.2%) of the specimen collected were culture positive. From the 142 positive patients, the proportion of bacterial isolates was higher in females 95(67%), than males 47 (33%). Out of 142 culture positive isolates, Eshcerchia coli (E.coli) 56 (39%), followed by Pseudomonas aeruginosa 35 (25%), Klebsiellae 24 (17%), Enterobacter 12 (8%), Citrobacter 8(6%), Acinetobacter 5(4%) and Serratia 2(1%).
Conclusion: E.coli followed by Pseudomonas aeruginosa, Klebsiellae, and Enterobacter were the most commonly isolated gram-negative bacteria. These bacteria were resistant to the routinely used antibiotics. Therefore, clinicians should practice rational choice of antibiotics and treatment should be guided by antimicrobial susceptibility testing.
References
c d c . g o v / h a i / o rg a n i s m s / g r a m - n e g a t i v e - bacteria.html. Gram-negative bacteria infections in Healthcare settings.
Tadesse BT, Ashley EA, Ongarello S, et al. Antimicrobial resistance in Africa: a systematic review. BMC Infect Dis 2017; 17(1): 616.
Farley E, Stewart A, Davies MA, et al. Antibiotic use and resistance: knowledge, attitudes, and perceptions among primary care prescribers in South Africa. S Afr Med J 2018; 108(9):763–771.
Tangcharoensathien V, Chanvatik S and Sommanustweechai A. Complex determinants of inappropriate use of antibiotics. Bull World Health Organ 2018; 96(2): 141–144.
Al Jarousha AM and Al Afifi A. Epidemiology and risk factors associated with developing bacterial meningitis among children in Gaza strip. Iran J Public Health 2014; 43(9):1176–1183.
Stone GS, Mitton J, Kenney J, et al. Global Health Informatics: Principles of eHealth and mHealth to Improve Quality of Care. MIT Press; 2017.
Lopez AD, Mathers CD, Ezzati M, et al. Global Burden of Disease and Risk Factors. The World Bank; 2006.
Shih JD, Wood LSY, Dambkowski CL, et al. An in vitro bacterial surface migration assay underneath sterile barrier material commonly found in a hospital setting. J Perinatol. 2017;37(7):848–852. doi:10.1038/jp.2017.28.
Schiavetti B, Wynendaele E, De Spiegeleer B. CIOMS Guide to vaccine safety communication. WHO Drug Inf. 2018;32(1).
Bailey&scott's diagnostic microbiology twelefth edition,Betty A.Forbes ,Daniel F.sahm,Alice s.weissfeld.
M a c k i e , M c C a r t n e y. p r a c t i c a l m e d i c a l microbiology.Collee JG, Fraser AG Marmion BP,Simmons A edts., 14 edn. Churchill and Livingstone.
Clinical and Laboratory Standards Institute (CLSI). Principles and Procedures for Blood Cultures; Approved Guideline. CLSI document M47-A. Wayne, PA: Clinical and Laboratory Standards Institute 2021.
Rossi F. The challenges of antimicrobial resistance in Brazil. Clin Infect Dis. 2011;52(9):1138–1143. doi:10.1093/cid/cir120.
Yitayeh L, Gize A, Kassa M, et al. Antibiogram profiles of bacteria isolated from different body site infections among patients admitted to GAMBY teaching general hospital Northwest Ethiopia. Infection and Drug resistance, 2021:14;2225-2232.
Demilie T, Beyene G, Melaku S, et al. Urinary bacterial profile and antibiotic susceptibility pattern among pregnant women in Northwest Ethiopia. Ethiop J Health Sci. 2012;22 (2):121–128.
Bischoff S, Walter T, Gerigk M, et al. Empiric antibiotic therapy in urinary tract infection in patients with risk factors for antibiotic resistance in a German emergency department. BMC Infect Dis. 2018;18(1):56. doi:10.1186/s12879-018-2960-9.
Krishna A, Chopra T. Active surveillance cultures for MRSA, VRE, multidrug-resistant gram-negatives. In: Infection Prevention. Springer; 2018:145–151.
Muluye D, Wondimenh Y, Ferede G, et al. Bacterial isolates and their antibiotic susceptibility patterns among patients with pus and/or wound discharge at Gondar University hiospoital. BMC Res Notes. 2014;7(1):619. doi:10.1186/1756-0500-7-619.
Tadvi J, Javedkar T.B, Bhavsar R, Garala N. Prevalence and antibiogram of P.aeruginosa at S.S.G. Hospital, Baroda, Gujarat, India. Journal of Research in medical and dental sciences, 2015;3(3):204-207.
Algun A, Arisoy, Gunduz T, et al. The resistance of Pseudomonas aeruginosa strains to fluoroquinolones group of antibiotics. Ind J Med Micro, 2004:22(2):112-14.
Peleg AY, Hooper DC. Hospital-acquired infections due to gram-negative bacteria. N Engl J Med. 2010;362 (19):1804-13. doi: 10.1056/NEJMra0904124.
Qin X, Hu F. Gastrointestinal carriage of Klebsiella pneumoniaeis a risk factor of subsequent hospital acquired infection. J EmergCrit Care Med.2017;1:47. doi: 10.21037/jeccm.2017.12.09.
Sahly H, Aucken H, Benedí VJ, Forestier C, Fussing V, Hansen DS, et al. Increased serum
resistance in Klebsiella pneumoniae strains producing extended-spectrum beta-lactamases.
A n t i m i c r o b A g e n t s C h e m o t h e r. 2004;48(9):3477-82. doi: 10.1128/AAC.48.9.3477-3482.2004.
WHO.int/news. WHO publishes list of bacteria for which new antibiotics are urgently needed. WHO official site, 27 February 2017.
Mustaq S, Javeid I, Hassan M. Antibiotic sensitivity pattern of Acinetobacter species isolated from clinical specimens in a tertiary care hospital. Biomedica, 2013;29:23-26.
Al-Mously N, Hakawi A. Acinetobacter baumannii bloodstream infections in a tertiary hospital: Antimicrobial resistance surveillance. Int J Infect Control, 2013;9(2):1-8.
Garcia-Garmendia JL, Ortiz-Leyba C, Garnacho-Montero J, et al. Risk factors for Acinetobacter baumanii Nosocomial bacteremia in critically ill patients: a Cohort study. Clin Infect Dis, 2001;33(7):939-46.
Silhavy T.J, Khane D, Walker S. The bacterial cell envelope. Cold spring Harb. Perspect. Boil., 2010;2a000414.
Ali S, Birhane M, Bekele S, Kirbu G, Teshagar L, Yilma Y, et al. Healthcare associated infection and its risk factor among patients admitted to a tertiary hospital in Ethopia: longitudinal study. Antimicro Resist Infect Control 2018;7:2.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Research Journal of Health Sciences

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Research Journal of Health Sciences journal is a peer reviewed, Open Access journal. The Journal subscribed to terms and conditions of Open Access publication. Articles are distributed under the terms of Creative Commons License (CC BY-NC-ND 4.0). (http://creativecommons.org/licences/by-nc-nd/4.0). All articles are made freely accessible for everyone to read, download, copy and distribute as long as appropriate credit is given and the new creations are licensed under the identical terms.





