Psychological correlates of stress among Nigerian high school adolescents during the third wave of COVID-19 Pandemic
Keywords:
COVID-19, third wave, stress, Nigerian adolescentsAbstract
Objective: The COVID-19 pandemic has significantly affected the mental health of adolescents. This study is aimed at determining the prevalence and psychological correlates of stress due to the COVID-19 pandemic among high school adolescents in Nigeria.
Methods: This is a cross-sectional descriptive online study involving 1008 Nigerian adolescents. Respondents completed study-specific sociodemographic questionnaire, Depression, Anxiety and Stress Scale– 21, Connor–Davidson Resilience Scale-10, Paediatric Quality of Life Enjoyment and Satisfaction, Insomnia Severity Index-7, Suicidal Behaviors Questionnaire-Revised, Drug Abuse Screening Test -10.
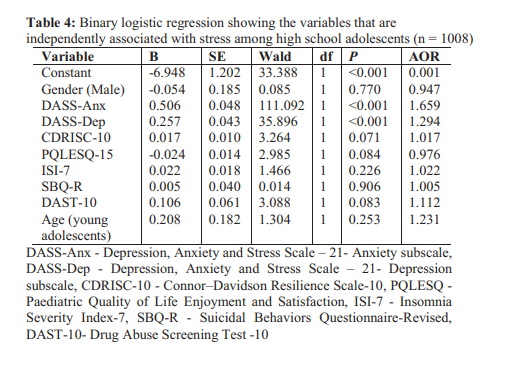
Results: The mean age of the respondents was 15.60 (SD 1.24) years. The prevalence of stress was 61.6%, while the prevalence of anxiety and depression was 57.4% and 50.8%, respectively. There were statistically significant positive correlations between stress and anxiety (rp = 0.669, P = <0.001), depression (rp = 0.612, P = <0.001), insomnia (rp =0.355, P =<0.001), suicidal tendencies (rp = 0.257, P = <0.001), drug abuse (rp = 0.251, P =<0.001) as well as between stress and age (rp = 0.129, P = <0.001). There was a statistically significant negative correlation between stress and quality of life (rp = -0.375, P = <0.001). The adolescents undergoing abnormal stress had higher odds of experiencing higher anxiety levels and depression.
Conclusion: Stress is associated with anxiety, depression, insomnia, substance abuse, suicidal behaviours, and reduced quality of life among Nigerian adolescents. Hence, there is a need to plan adolescent-centered mental health services during the COVID-19 pandemic.
References
Zhou SJ, Zhang LG, Wang LL, Guo ZC, Wang JQ, Chen JC, et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry. 2020;29(6):749-58.
Tang S, Xiang M, Cheung T, Xiang YT. Mental health and its correlates among children and adolescents during COVID-19 school closure: The importance of parent-child discussion. J. Affect. Disord. 2021;279:353-60.
Omari O, Sabei S, Rawajfah O, Abu SL, Aljohani K, Alomari K, et al. Prevalence and predictors of depression, anxiety, and stress among youth at the time of COVID-19: an online cross-sectional multicountry study. Depress Res Treat. 2020;2020.
Varma P, Junge M, Meaklim H, Jackson ML. Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: A global cross-sectional survey. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2021;109:110236.
Manzar MD, Albougami A, Usman N, Mamun MA. Suicide among adolescents and youths during the COVID-19 pandemic lockdowns: A press media reports-based exploratory study. J. Child Adolesc. Psychiatr. Nurs. 2021;34(2):13946.
Algahtani FD, Hassan S, Alsaif B, Zrieq R.
Assessment of the quality of life during COVID19 pandemic: A cross-sectional survey from the kingdom of Saudi Arabia. Int. J. Environ. Res. Public Health. 2021;18(3):847.
Coulombe S, Pacheco T, Cox E, Khalil C,
Doucerain MM, Auger E, et al. Risk and resilience factors during the COVID-19 pandemic: a snapshot of the experiences of Canadian workers early on in the crisis. Front. Psychol. 2020;11:3225.
Maggs JL. Adolescent life in the early days of the pandemic: less and more substance use. J Adolesc Health. 2020;67(3):307-8.
Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995;33(3):335-43.
Opakunle T, Aloba O, Opakunle O, Oyewole A, Osokoya O. Prevalence and correlates of obsessive–compulsive symptoms in a sample of undergraduate clinical medical students in Osogbo, Southwestern Nigeria. Niger. J. Health Sci. 2017;17(2):66.
Campbell-Sills L, Stein MB. Psychometric analysis and refinement of the connor–davidson resilience scale (CD-RISC): Validation of a 10-item measure of resilience. J Trauma Stress. 2007;20(6):1019-28.
Endicott J, Nee J, Yang R, Wohlberg C. Pediatric quality of life enjoyment and satisfaction questionnaire (PQ-LES-Q): reliability and validity. J Am Acad Child Adolesc Psychiatry. 2006;45(4):401-7.
Morin CM, Belleville G, Bélanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601-8.
Osman A, Bagge CL, Gutierrez PM, Konick LC, Kopper BA, Barrios FX. The Suicidal Behaviors Questionnaire-Revised (SBQ-R): validation with clinical and nonclinical samples. Assessment. 2001;8(4):443-54.
Skinner HA. The drug abuse screening test. Addict. Behav. 1982;7(4):363-71.
Campione-Barr N, Rote W, Killoren SE, Rose AJJ. Adolescent Adjustment During COVID-19: The
R o l e o f C l o s e R e l a t i o n s h i p s a n d
COVID-19-related Stress. J. Adolesc. Res. 2021;31(3):608-22.
Fazeli S, Zeidi IM, Lin C-Y, Namdar P, Griffiths MD, Ahorsu DK, et al. Depression, anxiety, and stress mediate the associations between internet gaming disorder, insomnia, and quality of life during the COVID-19 outbreak. Addict. Behav. Rep. 2020; 12:100307.
Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and
associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17(5):1729.
Rosen ML, Rodman AM, Kasparek SW, Mayes M, Freeman MM, Lengua LJ, et al. Promoting youth mental health during the COVID-19 pandemic: A longitudinal study. PLoS One. 2021;16(8):e0255294.
Gruber J, Prinstein MJ, Clark LA, Rottenberg J, Abramowitz JS, Albano AM, et al. Mental health and clinical psychological science in the time of COVID-19: Challenges, opportunities, and a call to action. Am Psychol. 2020. 2021;76(3):409-426.
Brown S, Doom J, Lechuga-Pena S, Watamura S, Koppels T. Stress and parenting during the global COVID-19 pandemic, child abuse and amp. Child Abuse Negl.2020; 2(6):104699.
Juma K, Wekesah FM, Kabiru CW, Izugbara CO. Burden, drivers, and impacts of poor mental health in young people of west and Central Africa: implications for research and programming. West African Youth Challenges and Opportunity Pathways: Palgrave Macmillan, Cham; 2020. p. 233-65.
Magson NR, Freeman JY, Rapee RM, Richardson CE, Oar EL, Fardouly J. Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. J Youth Adolesc. 2021;50(1):44-57.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Research Journal of Health Sciences

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Research Journal of Health Sciences journal is a peer reviewed, Open Access journal. The Journal subscribed to terms and conditions of Open Access publication. Articles are distributed under the terms of Creative Commons License (CC BY-NC-ND 4.0). (http://creativecommons.org/licences/by-nc-nd/4.0). All articles are made freely accessible for everyone to read, download, copy and distribute as long as appropriate credit is given and the new creations are licensed under the identical terms.

