Magnitude of limb loss attributable to diabetes mellitus in a tertiary institution in Nigeria
Keywords:
Diabetes, Diabetic foot ulcer, Amputation, Lower limb loss, Peripheral arterial diseaseAbstract
Background: Diabetes mellitus (DM) and its complications, continues to pose enormous challenge to
health and financial stability. Diabetes has remained a source of national and global economic burden. It
has been observed lately that incidence of diabetic foot ulcer (DFU); one of the complications of DM, is on
the increase and it is contributing hugely to financial loss, morbidity and mortality among diabetic
patients. This is taking a great toll on affected individuals in terms of cost of treatment, deformities
sustained, number of working/productive days lost while on admission and its attendant economic
implications, and ultimately mortalities recorded. The aim was to determine the magnitude of limb loss or
lower extremity amputation attributable to DM over a period of 12 months in tertiary institution and to
assess the clinical profile of the patients.
METHOD: This is a retrospective study of the records of all patients that were consecutively booked for
lower limb amputation and operated upon in the last 12 months at UNIOSUN Teaching Hospital, Osogbo,
South-Western Nigeria. Out of these total, cases of DFU were extracted to form another study group and
then studied in detail.
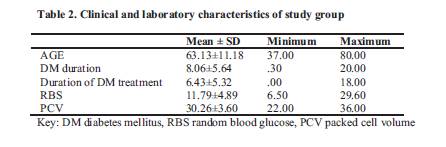
RESULTS; A total of 38 patients had lower limb amputation from July 2021 to May 2022. Twenty three of
the total number of amputations had DFU with a huge proportion of 60.5%, followed by road traffic
accident with 28.9% (n=11) Of the 23 diabetic cases , females were 15 with M:F ratio of 1:1.9. Mean age
was 63±11.18 years. Mean duration of DM was 8.06±5.64 years. 78.3% had no foot care education and
Doppler USS confirmed atherosclerosis in 100% of the patients. The commonest bacteria isolated was
Proteus 34.8%. Length of hospital stay ranged between 6 weeks to 16 weeks. Outcome of admission was
largely successful with 95.7% discharged and 4.3% mortality.
CONCLUSION: DFU contributes markedly to morbidity and mortality. Long duration of DM, presence
of PAD and DPN as well as advancement in age and wound infection with proteus bacterial are observed to
be risk factors associated with gangrenous DFU. However, larger studies are needed to establish these
factors as predictors of amputation in patient with DFU. Outcome was majorly good as majority of the
patients were discharged.
References
IDF Diabetes Atlas Tenth Edition 2021. Available at diabetesatlas.org > atlas > tenth edition
Uloko AE, Musa BM, Ramalan MA, Gezawa ID, Puepet FH, Uloko AT, et al. Prevalence and risk factors for diabetes mellitus in Nigeria: a systematic review and meta-analysis. Diabetes Ther. 2018;9(3):1307–16.
Olamoyegun M, Ibraheem W, Iwuala S, Audu M, Kolawole B. Burden and pattern of microvascular complications in type 2 diabetes in a tertiary health institution in Nigeria. Afr Health Sci. 2015;15(4):1136–1141.
Ekpebegh CO, Iwuala SO, Fasanmade OA, Ogbera AO, Igumbor E, Ohwovoriole AE. Diabetes foot ulceration in a Nigerian hospital: in-hospital mortality in relation to the presenting demographic, clinical and laboratory features. Int Wound J. 2009;6(5):381–385.
Jeffcoate WJ, Vileikyte L, Boyko EJ, Armstrong DG, Boulton AJM. Current challenges and opportunities in the prevention and management of diabetic foot ulcers. Diabetes care 2018; 41(4):645-652.
Ogbera AO, Fasanmade O, Ohwovoriole AE, Adediran O. An assessment of the disease burden of foot ulcers in patients with diabetes mellitus attending a teaching hospital in Lagos, Nigeria. Int J Low Extrem Wounds. 2006;(4):244-9.
Karam J, Shepard A, Rubinfeld I. Predictors of operative mortality following major lower extremity amputations using the National Surgical Quality Improvement Program public use data. J Vasc Surg. 2013;58(5):1276–824.
Lavery LA, Hunt NA, Ndip A, Lavery DC, Van Houtum W, Boulton AJ. Impact of chronic kidney disease on survival after amputation in individuals with diabetes. Diabetes Care. 2010;33(11):2365–2369.
Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. In Hypertension 2003;289(19):2560-2571.
Definition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycaemia: Report of a WHO/IDF Consultation. Geneva: World Health Organisation. 2006; 21.
Desmond D, Gallagher P. In: Quality of life in people with lower limb amputation. Handbook of disease burdens and quality of life measures. Preedy VR, Watson RR, editors. 2010. pp. 3785–3796.
Fasanmade O. A, Dagogo-Jack S. Diabetes care in Nigeria. Annals of Global Health 2015; 81(6):821–829.
Zhang Y, Lazzarini PA, McPhail SM, van Netten JJ, Armstrong DG, Pacella RE. Global disability burdens of diabetes‐related lower‐extremity complications in 1990 and 2016. Diabetes Care. 2020;43(5):964‐974.
Yesil S, Akinci B, Yener S, Bayraktar F, Karabay O, Havitcioglu H, et al. Predictors of amputation in diabetics with foot ulcer: single center experience in a large Turkish cohort. Hormones (Athens) 2009;8(4):286–295.
Rathur HM, Boulton AJ. The diabetic foot. Clin Dermatol. 2007;25(1):109–120.
Ugwu E, Adeleye O, Gezawa I, Okpe I, Enamino M, Ezeani I. Predictors of lower extremity amputation in patients with diabetic foot ulcer: findings from MEDFUN, a multi-center observational study. J Foot Ankle Res. 2019 June 14;12:34. doi: 10.1186/s13047-019-0345-y. PMID: 31223342; PMCID: PMC6570910.
McDermott MM, Greenland P, Liu K, Guralnik JM, Criqui MH, Dolan NC, Chan C, Celic L, Pearce WH, Schneider JR, et al. Leg symptoms in peripheral arterial disease: associated clinical characteristics and functional impairment. JAMA. 2001;286(13):1599–1606.
Lo ZJ, Surendra NK, Saxena A, Car J. Clinical and economic burden of diabetic foot ulcers: A 5-year longitudinal multi-ethnic cohort study from the tropics. Int Wound J. 2021;18(3):375-386. doi: 10.1111/iwj.13540. Epub 2021 Jan 26. PMID: 33497545; PMCID: PMC8244009.
Zhang P, Lu J, Jing Y, Tang S, Zhu BY. Global epidemiology of diabetic foot ulceration: a systematic review and meta‐analysis. Ann Med. 2017;49(2):106‐116.
Chinenye S, Young E (2011) State of Diabetes Care in Nigeria: A Review. The Nigerian Health Journal. 2011;11(4):101-106.
Okpe I, Ugwu E, Adeleye O, Gezawa I, Enamino M, et al. (2019) Foot Care Education, Health-Seeking Behaviour and Disease Outcome in Patients with Diabetic Foot Ulcer: Results from the Multi-Centre Evaluation of Diabetic Foot Ulcer in Nigeria Study. Int J Foot Ankle 3:038. doi.org/10.23937/2643-3885/1710038
Clayton W, Elasy TA. A review of the pathophysiology, classification, and treatment of foot ulcers in diabetic patients. Clin Diabetes. 2009;27(2):52–58.
Anyim O, Okafor C, Young E, Obumneme-Anyim I, C N. Pattern and microbiological characteristics of diabetic foot ulcers in a Nigerian tertiary hospital. Afri Health Sci. 2019;19(1). 1617-1627. https://dx.doi.org/10.4314/ahs.v19i1.37
Edo A, Edo G, Ezeani I. Risk factors, ulcer grade and management outcome of diabetic foot ulcers in a tropical tertiary care hospital. Niger Med J. 2013;54(1):59–63. doi: 10.4103/0300-1652.108900.
Guo S, Dipietro LA. Factors affecting wound healing. J Dent Res. 2010;89(3):219–229. doi: 10.1177/0022034509359125.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Research Journal of Health Sciences

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Research Journal of Health Sciences journal is a peer reviewed, Open Access journal. The Journal subscribed to terms and conditions of Open Access publication. Articles are distributed under the terms of Creative Commons License (CC BY-NC-ND 4.0). (http://creativecommons.org/licences/by-nc-nd/4.0). All articles are made freely accessible for everyone to read, download, copy and distribute as long as appropriate credit is given and the new creations are licensed under the identical terms.

