High level of perceived stress among essential workers during the COVID 19 lockdown in a Nigerian state
Keywords:
Essential workers, lockdown, High Perceived Stress, Ekiti State, NigeriaAbstract
Background: COVID-19 pandemic caused unexpected socio-economic changes globally. This study determined the prevalence and factors associated with perceived stress among essential workers during the COVID-19 lockdown in Ekiti State, Nigeria.
Method: A cross-sectional descriptive study that involved 588 essential workers in Ekiti State, Nigeria during the COVID-19 lockdown. The Perceived Stress Scale was used in the study Chi-square test of statistical significance and multivariate analysis using binary logistic regression were used in the analysis and the level of statistical significance was determined by a p-value of <0.05.
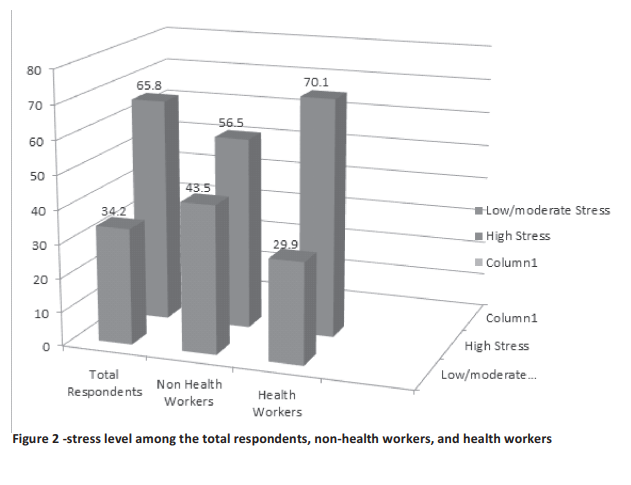
Results: The prevalence of high perceived stress levels among all the respondents, health workers, and non-health workers were 64.1% (63.3-70.6), while health workers and non-health workers had a prevalence of 70.1% (65.5 -73.3) and 56.5% (23.5-38.7) respectively. The majority of the respondents related their sources of stress to inadequate transportation (63.3%), hearing of COVID related news (47.4%), and lack of finance (55.1%). Using Logistic Regression respondent respondents who were not satisfied with the support they received from the government during the pandemic had three fold high stress levels than respondents who were satisfied with the support received from the government [AOR= 3.228, (CI= 1.771- 5.886)]. Furthermore, the odd of the high stress level was one fold increased among male respondents than female respondents [AOR = 1.08 CI= (1.410-6.215).
Conclusion: Stress management is recommended given the high-stress level among essential workers.
References
Bansal P, Bingemann TA, Greenhawt M, Mosnaim G, Nanda A, Oppenheimer J, et al. Clinician wellness during the COVID-19 pandemic: extraordinary times and unusual challenges for the allergist/immunologist. The Journal of Allergy and Clinical Immunology: In Practice. 2020;8(6):1781-90.
Al-Hanawi MK, Mwale ML, Alshareef N, Qattan AM, Angawi K, Almubark R, et al. Psychological distress amongst health workers and the general public during the COVID-19 pandemic in Saudi Arabia. Risk management and healthcare policy. 2020;13:733-742.
Del Rio C, Malani PN. COVID-19—new insights on a rapidly changing epidemic. Jama. 2020;323(14):1339-40.
Nas FS, Ali M, Azu LM, Abdallah MS, Yusuf SF. Epidemiology of novel COVID-19 in Nigeria. Microbes and Infectious Diseases. 2020;1(2):4956.
Roy RK, Roy DK, Goit RK. Substance Abuse Among Medical Students–A Survey in a Medical College in Nepal. Journal of Nepalgunj Medical College. 2018;16(1):71-5.
Kim Y, Calzada EJ, Barajas-Gonzalez RG, Huang K-Y, Brotman LM, Castro A, et al. The role of authoritative and authoritarian parenting in the early academic achievement of Latino students. Journal of Educational Psychology. 2018;110(1):119.
Felice C, Di Tanna GL, Zanus G, Grossi U. Impact of COVID-19 outbreak on healthcare workers in Italy: results from a national e-survey.
Journal of community health. 2020
Aug;45(4):675-83
Cooper A-P, Jormanainen I, Shipepe A, Sutinen E. Faith communities online: Christian churches' reactions to the COVID-19 outbreak.
International Journal of Web-Based
Communities. 2021;17(2):99-119.
Bingemann T, Sharma H, Nanda A, Khan DA, Markovics S, Sussman J, et al. AAAAI Work Group Report: physician wellness in allergy and immunology. The Journal of Allergy and Clinical Immunology. 2020;8(4):1224-9.
Biswas P, Chatterjee S. Hand hygiene compliance among doctors in a tertiary care hospital of India. The Indian Journal of Pediatrics. 2014;81(9):967-8.
Luan R, Pu W, Dai L, Yang R, Wang P.
Comparison of psychological stress levels and associated factors among healthcare workers, frontline workers, and the general public during the novel coronavirus pandemic. Frontiers in Psychiatry. 2020;11: 583971- 583976
Khasne RW, Dhakulkar BS, Mahajan HC,
Kulkarni AP. Burnout among healthcare workers during COVID-19 pandemic in India: results of a questionnaire-based survey. Indian Journal of Critical Care Medicine: Peer-reviewed, Official Publication of Indian Society of Critical Care Medicine. 2020;24(8):664-671.
Omilusi M, Isaac AA. From 200 Dollars to 50 Dollars: The Political Economy of Nigerian Workers' Retrogressive Living Wage in Four Decades. I nternational Journal of Research in
Business and Management; 2020;2(1); 1-11
Ganiyu KA, Ekwueme MC, and Ebiware-Otubo A. Completeness and Legibility of
Prescriptions and Prescribing Practice at Two Health Centres on Wilberforce Island, Bayelsa State, Nigeria. Journal of Basic and Social Pharmacy Research, 2020;1(4):24-32.
Shapiro AJ, Heath NL, Carsley D. Pilot evaluation of the feasibility and acceptability of StressOFF Strategies: a single-session schoolbased stress management program for
adolescents. Advances in School Mental Health Promotion. 2016;9(1):12-28.
Ojobo HI, Malaysia UT, Malaysia UT, Malaysia
UT. Validating the Measures of Perceived Restorativeness in Obudu Mountain Resort, Cross River State, Nigeria. Open Journal of Social Sciences. 2014;2(11):1-6
James BO, Thomas IF, Omoaregba JO, Okogbenin EO, Okonoda KM, Ibrahim AW, Salihu AS, Oshodi YO, Orovwigho A, Odinka PC, Eze GO, Onyebueke GC, Aweh BE.
Psychosocial correlates of perceived stress among undergraduate medical students in Nigeria. International Journal of Medical Education. 2017; 26;(8):382-388.
18 Ossai EN, Alo AT, Onwe BC, Okoro DO, Ezeagu NE, Ogbonnaya LU. Prevalence and predictors of perceived stress: A study among medical students of Ebonyi State University Abakaliki, Nigeria. Asian Journal of Advanced Research and Reports. 2019; 4:1-9.
Ufua DE, Osabuohien E, Ogbari ME, Falola HO, Okoh EE, Lakhani A. Re-strategising government palliative support systems in tackling the challenges of COVID-19 Lockdown in Lagos State, Nigeria. Global Journal of Flexible Systems Management. 2021
Jun;22(1):19-32.
Shan C, Tang D Y. The value of employee satisfaction in disastrous times: Evidence from COVID-19. Available at SSRN 3560919. 2020. 1-42
Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA network open. 2020;3(3):203976-2033988
Si M-Y, Su X-Y, Jiang Y, Wang W-J, Gu X-F, Ma L, et al. Psychological impact of COVID-19 on medical care workers in China. Infectious diseases of poverty. 2020;9(1):1-13.
Aiyer A, Surani S, Varon J, Ali M, Sunesara S. Covid-19 Anxiety and Stress Survey (Cass) in
Healthcare Workers Due To Coronavirus Disease 2019. Chest. 2020;158(4):313-315
Sathiya N, Ruwaidha R, Nusrath FS, Fathima F, Gomathy T, Shailendra HK. Perceived stress levels and their sources among doctors and nurses working in a tertiary care teaching hospital, Kancheepuram, Tamil Nadu. Ntl J Community Med. 2016;7(7):603-8.
Lindo J, LaGrenade J, McCaw-Binns A,
Eldemire-Shearer D. Health status and health maintenance practices among doctors and nurses at two hospitals in Jamaica. West Indian medical journal. 2009;58(6).539-546
Lindo J, McCaw-Binns A, LaGrenade J, Jackson M, Eldermire-Shearer D. Mental well-being of doctors and nurses in two hospitals in Kingston, Jamaica. West Indian Med J. 2006;55(3):153-9.
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Research Journal of Health Sciences

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Research Journal of Health Sciences journal is a peer reviewed, Open Access journal. The Journal subscribed to terms and conditions of Open Access publication. Articles are distributed under the terms of Creative Commons License (CC BY-NC-ND 4.0). (http://creativecommons.org/licences/by-nc-nd/4.0). All articles are made freely accessible for everyone to read, download, copy and distribute as long as appropriate credit is given and the new creations are licensed under the identical terms.

