Sun-protection strategies amongst people living with Albinism in Benin-city, Southern Nigeria
Keywords:
Oculocutaneous albinism, sun-protectionAbstract
Background: Oculocutaneous albinism (OCA) is an inherited disorder of generalized hypopigmentation. Dermatological care and protection from UV radiation are necessary for individuals with OCA. We assessed the patterns of protection strategies amongst persons living with albinism in Benin-city, Nigeria.
Methods: Snow ball sampling methods were employed to investigate sun protection strategies amongst albinos in UBTH, Benin-city, Nigeria. Avoidance of sun peak hours, sun-protection clothing and sunscreen preparations used were analyzed during semi-structured face to face interviews conducted in the outreach clinics.
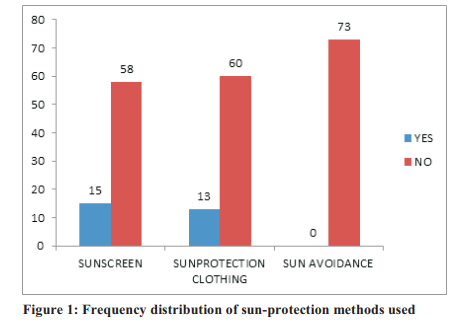
Results: A total of 73 participants living with albinism were studied. The mean age of the participants was 24.1years± 11.3 years. The predominant activity type was out-door occurring in 62(84.9%) of the population observed. Participants with albinism in this study were exposed to high levels of ultraviolet radiation throughout the year. They all reported being unable to avoid sun-peak hours. Sunscreens were used in 15 (20.5%) albinos studied while sun-protection clothings were worn in 13(17.8%) respondents. Sunscreens were used more in those who engaged principally in out-door activities. This was observed in 10(13.7%) clients studied (p=0.04).
Conclusion: People leaving with albinism who attended UBTH outreach skin clinic had insufficient sun protection strategies.
References
Spritz RA. Detection of mutations in tyrosinase gene in a patient with type 1A oculocutaneous albinism. N Engl J Med 1990; 322:17224-28
King RA. Temperature sensitive tyrosinase associated with peripheral pigmentation in oculocutaneous albinism. J Clin Invest 1991; 87: 1046-53
Wei ML. Hermansky-pudlak syndrome: A disease of protein trafficking and organelle function. Pigment call Rev 2006; 19: 19-42
Venter PA, Christianson AL, Hutamo CM, MP M,
GS G: Congenital anomalies in rural black South African neonates – a silent epidemic?. S Afr Med J. 1995, 85 (1): 15-20.
Lund P, Maluleke T, Gaigher I, Gaigher M: Oculocutaneous albinism in a rural community of South Africa: A population genetic study. Annals of Human Biology. 2007, 34 (4): 493-497.
Bothwell JE, Abs T: Pigmented skin lesions in tyrosinase-positive oculocutaneous albinos: A study in black South Africans. International Journal of Dermatology. 1997, 36 (11): 831-836.
Kromberg JG, Castle D, Zwane EM, Jenkins T: Albinism and skin cancer in Southern Africa. Clin Genet. 1989, 36 (1): 43-52.
Yakubu A, Mabogunje OA: Skin cancer in African albinos. Acta Oncologica. 1993, 32 (6): 621-622.
Gaigher R, Lund P, Makuya E: A sociological study of children with albinism at a special school in the Limpopo province. Curationis. 2002, 25 (4): 4-11.
Luande J, Henschke C, Mohammed N: The Tanzanian human albino skin. Natural history. Cancer. 1985, 55 (8): 1823-1828.
Preston D, Stern R: Nonmelanoma cancers of the skin. The New England Journal of Medicine. 1992, 327 (23): 1649-1662.
Okulicz JF, Shah RS, Schwartz RA, Janniger CK: Oculocutaneous albinism. Journal of the European Academy of Dermatology and
Venereology. 2003, 17: 251-256.
Asuquo M, Agweye P, Ugare G, Ebughe G: Basal cell carcinoma in five albino Africans from the south-eastern equatorial rain forest of Nigeria. International Journal of Dermatology. 2007, 46 (7): 754-756.
Okoro A: Albinism in Nigeria. A clinical and social study. The British Journal of Dermatology. 1975, 92 (5): 485-492.
Lookingbill DP, Lookingbill GL, Leppard B. Actinic damage and skin cancer in albinos in northern Tanzania: findings in 164 patients enrolled in an outreach skin care program. Journal of the American Academy of Dermatology. 1995, 32 (4): 653-658.
Jekel JF, Elmore JG, Katz DL. Sample size, randomization and probability theory. Epidemiology, Biostatistics and Preventive Medicine. Philadelphia: Saunders; 1996; 159-71.
Snow ball sampling- Chain referral sampling. Available at explorable.com/snowball sampling. (Cited on 29th January 2014 at 23.50hrs)
Hong E, Zeeb H, Repacholi M: Albinism in
Africa as a public health issue. BMC Public
Health. 2006, 6 (1): 212-10.1186/1471-2458-6212.
How to cite this article:
Taylor J, Lund P: Experiences of a feasibility study of children with albinism in Zimbabwe: A discussion paper. Int J Nurs Stud . 2008, 45 (8): 1247-1256.
Lund PM: Health and education of children with albinism in Zimbabwe. Health Education
Research. 2001, 16 (1): 1-7. 10.1093/her/16.1.1.
Kagore F, Lund PM. Oculocutaneous albinism among school children in Harare, Zimbabwe. Journal of Medical Genetics.1995; 32:859–861
Adam J, Samdani I, Bahram K. A unique albino village of Bhatti tribe in rural Sindh, Parkistan, with occulocutaneous albinism manifestation. An epidemiological study. Iranian Journal of dermatology 2009; 12:2
Kromberg JG, Castle D, Zwane EM, Jenkins T: Albinism and skin cancer in Southern Africa. Clin Genet. 1989; 36:43-52.
Clydesdale G, Dandie H. Ultraviolet light induced injury: immunological and inflammatory effects. Immunology and cell biology 2001; 79(6):547-68.
Hanneman K, Cooper K, Baron E: Ultraviolet
immunosuppression: mechanisms and
consequences. Dermatologic Clinics. 2006, 24 (1): 19-25.
Naylor M, Farmer K. The case for sun screen.A review of its use in preventing actinic damage and neoplasia. Arch dermatol 1997; 33(90):1146-54.
Levy SB. How high is SPF?. Arch dermatol1995;
(12):1463-4
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Research Journal of Health Sciences

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Research Journal of Health Sciences journal is a peer reviewed, Open Access journal. The Journal subscribed to terms and conditions of Open Access publication. Articles are distributed under the terms of Creative Commons License (CC BY-NC-ND 4.0). (http://creativecommons.org/licences/by-nc-nd/4.0). All articles are made freely accessible for everyone to read, download, copy and distribute as long as appropriate credit is given and the new creations are licensed under the identical terms.

