A Cross-sectional Study of Female HIV Patient Perspective of Dyadic Adjustment in HIV Sero-concordant and Sero-discordant couples
Keywords:
Couple, Distress, Dyadic adjustment, HIV, Sero-concordant, Sero-discordantAbstract
Background: Dyadic Adjustment is defined as the process with which couples form a steady relationship. This study assessed dyadic adjustment in HIV couples in Ogun State, Nigeria.
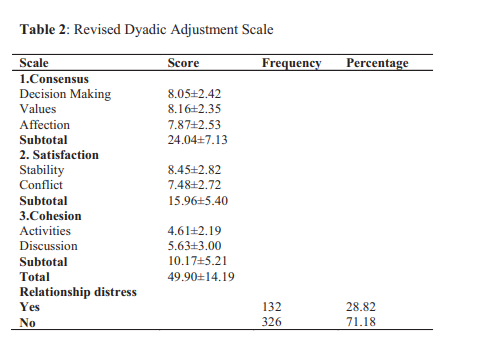
Methods: This cross sectional study was carried out among 458 women accessing HIV care in tertiary hospitals in Ogun State, Nigeria. Participants were evaluated using the Revised Dyadic Adjustment Scale and analyzed using the Stata/SE 15.1 statistical Package. Chi-square and t-tests were used to determine the correlates of dyadic adjustment (Distress/Non-distress) while logistic regression was used to determine the predictors of distress.
Results: Only 28.82% had relationship distress while the majority (71.18%) had no distress. There was a statistically significant association between marital status and the level of distress. Those who were currently married were less likely to have distress than those who were single or previously married.
Conclusion: Those who were not married were more predisposed to distress. More support for these groups is therefore recommended.
References
Largu A, Manciuc C, Vata A, Nicolau C, Prisacaru L, Clubotaru F et al. Dyadic adjustment in HIV seroconcordant and serodiscordant couples. Rev Med Chir Soc Med Nat, lasi. 2012; 116(3): 718-
Locke HJ, Wallace EM. Short marital adjustment and prediction tests: Their reliability and validity. J Mar Fam Living. 1959; 21(3): 251-55
Leanne KL Marital adjustment among rural couples: The role of expressiveness .Sex Roles 1989; 21: 579-590
Ayres J. Strategies to maintain relationships: Their identification and perceived usage. Communication Quarterly.1983; 31:62– 67
Canary D, Stafford L and Semic BA. A panel study of the associations between maintenance strategies and relational characteristics. Journal of Marriage and Family. 2002; 64: 395– 406.
Guerrero LK, Eloy SV and Wabnik AI. Linking maintenance strategies to relationship development and disengagement: A reconceptualization. Journal of Social & Personal Relationships. 1993; 10: 273–283
Spanier GB. Manual for the Dyadic adjustment Scale. North Tonawanda, NY. A multi-health system; 1989.
Vamos S, Cook R, Chitalu N, Mumbi M, Weiss SM, Jones D. Quality of relationship and sexual risk behaviors among HIV couples in Lusaka, Zambia. AIDS Care. 2013; 25(9): 1102- 8
Sales JM, Lang DL, Di-Clement RJ, Latham TP, Wingood GM, Hardin JW et al. The mediating role of partner communication frequency on condom use among African American adolescent females participating in an HIV prevention intervention. Health Psychole. 2012; 31(1):63-9.
Marfatia YS, Naik E, Singhai P, Naswa S. Profile of HIV seroconcordant/discordant couples a clinic-based study at Vadodara, India. Indian J Sex Transm Dis AIDs. 2013; 34(1): 5-9
Warren JT, Harvey SM, Agnew CR. One Love; Explicit monogamy agreements among
heterosexual young adult couples at increased risk of sexually transmitted infections. J Sex Res. 2012; 49(2-3): 282-9
Marlow HM, Tolley EE, Kohl R, Mehendale S. Sexual communication among married couples in the context of a microbicide clinical trial and acceptability study in Pune, India. Cult Health Sex. 2010; 12(8): 899-912
Njau B, Watt MH, Ostermann J, Manongi R, Sikkema KJ. Perceived acceptability of homebased couples voluntary HIV counseling and testing in northern Tanzania. AIDS Care. 2012; 24(4): 413-9
Swan H and O'Connell DJ. The Impact of Intimate Partners Violence on women's condom
negotiation efficacy. J Interpers Violence. 2012; 27(4): 775-92
Gilling- Smith C, Nicopoullos JD, Semprini AE, Frodsham LC. HIV and reproductive care; a review of current practice. BJOG. 2006;113(8) :869-78
Martins A, Alves S, Chaves C. Prevalence and factors associated with fertility desires/intentions among individuals in HIV-serodiscordant relationships: a systematic review of empirical studies. J Int Aids So. 2019; 22: e25241
Mmeje O, Cohen CR, Murage A, Ong'ech J,
Kiarie J, Van der Poel S. Promoting reproductive options for HIV affected couples in sub-Saharan Africa. BJOG. 2014; 121(5): 79-86
Ogun State Nigeria Population Statistics Charts, Map and Location. Available at . Accessed on 20/06/12
Ogun State. Health Facility Listing in Ogun State.
A v a i l a b l e a t www.library.procurementmonitor.org.files. Accessed on 12/06/18
Cochran WG. Sampling Techniques. 2nd ed.. New York: John Wiley and Sons, Inc.; 1963
Osinde MO, Kaye DK, Kakaire O. Intimate partners' violence among women with HIV infection in rural Uganda: critical implications for policy and practice. BMC women's Health. 2011; 11(1): 50
Caravelli L, Lubrano-Lavadera A, Malagoli Togliatti M. T08-P-01 Communication patterns and dyadic adjustment of couples: a preliminary study. Sexologies 2008; 17(1):S112
Ramlagan S, Matseke G, Rodriguez VJ, Jones DL, Peltzer K, Ruiter RAC et al. Determinants of disclosure and non-disclosure of HIV-positive status, by pregnant women in rural South Africa. Sahara J 2018; 15(1): 155-163 24. Hallberg D, Kimarion TD, Mtuya C, Msuya M, Bjorling G. Factors affecting HIV disclosure among partners in Morongo, Tanzania. Int J Afr Nurs Sc 2019; 10:49-54
Amoran OE. Predictors of disclosure of serostatus to sexual partners among people living with HIV/AIDS in Ogun State, Nigeria. Nigerian Journal of Clinical Practice. 2012; 15(4): 385-90
Odiachi A, Erekaha S, Cornelius LJ, Isah C, Ramadhani HO, Rapoport L et al. HIV status disclosure to male partners among rural Nigerian women along with the prevention of mother to child transmission of HIV cascade: a mixedmethods study. BMC Reprod Health. 2018; 15(1): 36
Dunkle KL, Stephenson R, Karita E, Chomba E,
Kayitenkore K, Vwalika C et al. New
Heterosexually Transmitted HIV Infections in Married or Cohabiting Couples in Urban Zambia and Rwanda: an analysis of Survey and Clinical Data. Lancet. 2008; 371(9631): 22183-91
Brubaker S, Bukusi E, Odoyo J, Achando J, Okumu A, Cohen CR. Pregnancy and HIV transmission among HIV discordant couples in a clinical trial in Kisumu, Kenya. HIV Med. 2011;12(5): 316-21
Greeff M, Phetlhu R, Makoae LN. Disclosure of HIV Status: experiences and perceptions of persons living with HIV/AIDS and nurses involved in their care in Africa. Qual Health Res. 2008; 18(3): 311-24.
Ncama BP, Mclnerney PA, Bhengu BR. Social Support and medication adherence in HIV disease in Kwazulu-Natal, South Africa. Int J Nurs Stud. 2008; 45(12):1757-63
Fitzpatrick MA and Best P. Dyadic Adjustment in Relational Types: Consensus, Cohesion, Affectional Expression, and Satisfaction in
Enduring Relationships. Communication Monographs. 1979; 46:167-178
Darghouth S, Brody L, Alegria M. Does Marriage Matter? Marital status, Family Processes, and Psychological Distress among Latino men and women. Hispanic J Behav Sci. 2015; 37(4):482-
Hope S, Rodgers B, Power C. Marital status transitions and psychological distress: longitudinal evidence from a national population sample. Psychol Med. 1999; 29(2): 381-9
Choi NG, Jung-Hwa Ha. Relationship between spouse/partner support and depressive symptoms in older adults: Gender difference. Aging Ment
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Research Journal of Health Sciences

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Research Journal of Health Sciences journal is a peer reviewed, Open Access journal. The Journal subscribed to terms and conditions of Open Access publication. Articles are distributed under the terms of Creative Commons License (CC BY-NC-ND 4.0). (http://creativecommons.org/licences/by-nc-nd/4.0). All articles are made freely accessible for everyone to read, download, copy and distribute as long as appropriate credit is given and the new creations are licensed under the identical terms.

