Management of snakebite victims using low dose antisnake venom in a tertiary hospital in Southern Nigeria: A 5-year Retrospective study
Keywords:
Snake bite, envenomation, polyvalent antisnake venom, NigeriaAbstract
Objective: Antisnake venom (ASV) is a specific antidote for the management of snake bite envenomations. This study profiled the treatment and outcome of adult snake bite victims managed using low dose antisnake venom.
Methods: This was a 5-year retrospective study that involved all adult patients who presented in University of Benin Teaching Hospital, Benin City, Nigeria, with a history of snake bite. Information obtained were demographic characteristics, clinical features, and administered treatment per established. All patients with a diagnosis of snake bite envenomation were administered ASV.
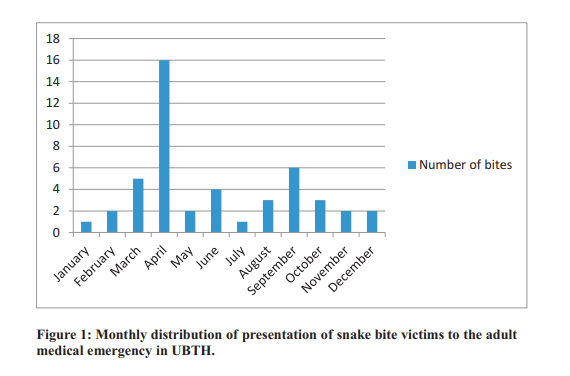
Results: Sixty patients were seen during the study period, 35(58.3%) males, 25(41.7%) females with a mean age was 34.7±13.3. The mean time from bite to presentation was 14.67±14.05 hours with range of 148 hours. Twenty patients (33.3%) had snake bite envenomations, of these eleven (57.9%) were managed and discharged after administration of 30 to 40 mls of polyvalent ASV. The mean dose of PASV used was 3.9 ± 2.0 vials. The most encountered clinical indication for ASV administration was progressive painful swelling. No death was recorded throughout this period studied.
Conclusion: Adoption of the low dose regimen in the management of snake bite envenomations may be as effective as the traditional high dose regimen.
References
W H O . S n a k e b i t e . http://www.who.int./neglected_disease/diseases/ Snakes bites/en/index.html (Accessed Sept 22, 2017).
Chippaux JP. Estimate of the burden of snake bite in Sub-Saharan Africa. Toxicon 2011, 57(4): 586599.
Warrel DA. Snake bite. Lancet 2010; 375:77-88.
Omogbai EKI, Nworgu ZAM, Imhafidon MA, Ikpeme AA, Ojo DO, Nwako CN. Snake bites in Nigeria: A study of the prevalence and treatment in Benin City. Trop J Pharm Res. 2002;1(1): 3944.
Blaylock R. Epidemiology of snake bite in
Eshowe, Kwazulu-Natal, South Africa. Toxicon 2004; 43 (2): 159-166.
Cherian AM, Girish TS, Jagannati M, Lakshmi M. High or Low - A trial of low dose Antisnake venom in the treatment of poisonous snake bites. J Assoc Phys India 2003;61: 387-390.
Gadwalkar SR, Kumar NS, Kushal DP, Shyamala G, Mohammad MZ, Vishwanatha H et al.
Judicious use of antisnake venom in the present period of scarcity. Indian J Crit Care Med 2014; 18 (11): 722-727.
Ranjan Das R, Sanker J and Dev N. High dose versus low dose antivenom in the treatment of poisonous snake bite: A Systematic Review. India J Crit Care Medicine 2015; 19(6): 340-349.
Pugh RNH and Theakston RDG. Incidence and mortality of snakebites in Savannah Nigeria.
Lancet1980; 2: 1181-3.
Coleman J.J, Kafle K.K, Ferner RE. Emergency Medicine: Snake bite poisoning. In Drug Benefits and Risk; CH 32, p 515. Ed. Van Bextel C.J, Santoso B, Edward I.R. Uppsala Monitoring Centre, IOS press, Amsterdam. Washington DC
Chippaux P, Vieillefosse S, Sali O, Mafouta R,
Diallo A. Appraisal of snake bite incidence in Senegal, West Africa. Bull Soc Patho Exot 2005; 98 (4): 277-282.
Habib AG, Lamorde M, Dalhat MM, Habib ZG. Cost-effectiveness of Antivenoms for snake bite envenoming in Nigeria. PLoS Negl Trop Dis
; 9 (1): 1-7.
Gutierrez JM, Williams D, Fan HW, Warrell DA.
Snake bite envenoming. Toxicon 2010; 56:12231235.
WHO. Guidelines for the prevention and clinical management of snake bite in Africa. WHO
Regional Office for Africa, Brazzaville.2010.
Vijay KAB, Gudge S, Mithare S, Mudbi S,
Kulkarni S. A trial of low dose antisnake venom in the treatment of poisonous snake bites in Brims Teaching Hospital Bidar. Journal of Evolution of Medical and Dental Sciences 2014, 3(30): 85448551.
Warrell DA. Treatment of bites by adders and exotic venomous snakes. BMJ 2005; 331(7521):
-1247.
Wood D, Webb C, and DeMeyer J. Severe snakebites in northern Kwazulu-Natal: Treatment modalities and outcome. S Afri Med J 2009; 99:
-818.
Habib AG and Warrell DA. Antivenom therapy of carpet viper envenoming; Effectiveness and Strategies for delivery in West Africa. Toxicon 2013; 69, 82-89.
Srimannarayana J, Dutta TK, Sahai A, Badrinath S. Rational use of ASV; Trial of various regimens in Haematotoxic snake envenomation. J, Assoc Phys India 2004; 52: 788-793.
Agarwal R, Aggarwal AN, Gupta D, Behera D, Jundal Sk. Low dose of Antisnake venom is as effective as high dose in patients with severe neurotoxic snake envenoming. Emerg Med J 2005;22: 397-399.
Livinus Hindi. Scared of death, over 4000 snakebite victims resort to self help. Punch Newspapers. 2017. Available from http: // punchng.com/ scared-of-death-over-400-snakebite victimsresort-to-self help/ ( Accessed 11th November 2017).
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Research Journal of Health Sciences

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Research Journal of Health Sciences journal is a peer reviewed, Open Access journal. The Journal subscribed to terms and conditions of Open Access publication. Articles are distributed under the terms of Creative Commons License (CC BY-NC-ND 4.0). (http://creativecommons.org/licences/by-nc-nd/4.0). All articles are made freely accessible for everyone to read, download, copy and distribute as long as appropriate credit is given and the new creations are licensed under the identical terms.

