Estimation of zinc levels among children with malnutrition at Usmanu Danfodiyo University Teaching Hospital, Sokoto, Northwestern Nigeria
Keywords:
zinc, malnutrition, SokotoAbstract
Objective: Zinc plays a critical role in many body functions and its deficiency is associated with impaired cognitive function, behavioral problems, memory impairment, growth retardation, increased incidence of diarrhoea and recurrent infections. Although severe zinc deficiency is not common, mild to moderate deficiency is quite common globally. It is estimated that some form of zinc deficiency affects about one third of the world population, with estimates ranging from 4% to 73% across sub Saharan Africa. To determine the prevalence of zinc deficiency among malnourished children at Usmanu Danfodiyo University Teaching Hospital (UDUTH), Sokoto.
Methods: Study was descriptive cross-sectional, carried out at the Paediatric department of UDUTH, Sokoto from April 2013 to June 2014. It was conducted among children aged between 6 and 60 months who presented to the OPD and those that were admitted into paediatric wards of UDUTH with malnutrition. Children with similar characteristics that were well nourished served as controls. Cohorts were recruited consecutively until the required sample size was obtained. 5mls of venous blood was taken for serum zinc analysis from each child.
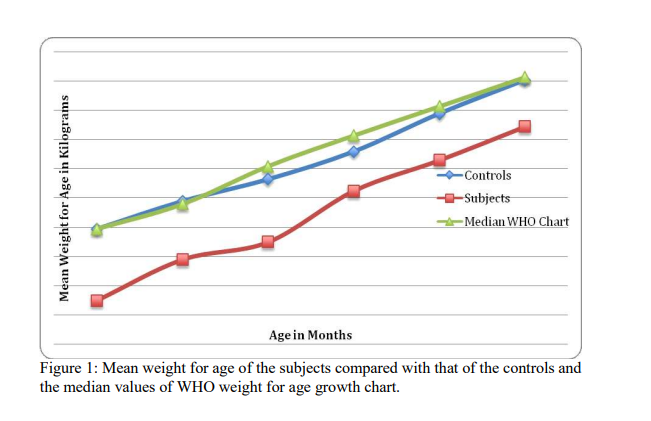
Results: A total of 550 children were studied with 275 apiece for cohorts. The mean age of the malnourished children was 26.2±14.6 months compared to 28.2±17.0 months recorded for the controls (p=0.157).The mean serum zinc levels for the study subjects 13.5±3.3µmol/L was significantly lower than that of the controls (15.8±1.9µmol/L) (t=9.42, df=548, p=0.0001).
Conclusion: The prevalence of zinc deficiency among both malnourished children and the controls was 0% using WHO reference value for children below the age of 5 years. Prophylactic doses of zinc should be given in all malnourish children in situation where mineral mix is not added to feed or f75 and f100 are not available. There is need to adhere to and use recommended cut off values recommended by WHO for defining zinc deficiency by researchers.
References
Ahmed T, Michaelsen KF, Frem JC and
Tumvine J. Malnutrition Report of the
FISGHAN Working Group. J Pediatr
Gastroenterol Nutr 2012;55:626 -31.
UNICEF. Improving child nutrition. The achievable imperative for global progress. New York, UNICEF 2013.
World hunger problems facts, figures and s t a t i s t i c s a v a i l a b l e a t h t t p / / www.worldhunger.org>2015-world-hun accessed online 15th September 2016.
Oyedeji G.A. Is it well with the Nigerian child? Obafemi Awolowo University Ile Ife, Nigerian inaugural lecture series 171. 2000; 13
UNICEF State of the World's children: Official publication of the United Nations. 2005; 85-8.
Reddy V. Protein-Energy Malnutrition. In: Stanfield P. Diseases of children in the subtropics and tropics 4th ed.1991; 335-57.
Pius CM, Josephat MC, Agozie U, Herbert AO, Odutola O and Aworene TC. Prevalence of malnutrition among pre-school children in South-east Nigeria. Ital J pediatr 2014;40:75.
Lawoyin TO. Risk factors for infant mortality in a rural African community. J Roy Soc Health 2000; 121:114-8.
Gomez F. Malnutrition in Infancy and Childhood with Special Reference to
Kwashiorkor. In: Levine ed. Advances in Paediatrics. New York Yearbook 1955; 7:131-
Ohiokpehal O, Mbithe DD, Kamau J. Serum zinc levels of School children on a corn soy blend feeding trial in primary school in Suba district Kenya, tropical soil biology and fertility, available at www.biosciencies,elewa.org, accessed 14th September 2016.
Hatz C and Brown KH. Assessment of the risk of zinc deficiency in population and options for its control. Food and Nutr Bull 2004; 25:10:91-204
Farhan J, Aneela A, Saifullah S, Mohammed A, Nadeem H, Bushra A. Comparison of serum zinc levels between healthy and malnourished children. A.P.M.C 2009; 3 (2): 139-142
Savitri T, Neela G, Poonan K. Serum Copper and zinc concentration and their relation to superoxide dimutase in severe malnutrition. Eur J paed 2004; 163:742-744
Debayo MB. Zinc. In: Handbook of clinical chemistry, Spectrum Books limited Ibadan, 2nded. 2006; 665-667
David BM. Zinc. In: Tiez Fundamental of
Clinical Chemistry, 5th edition: 2004; 578- 83
Anuradha J, Meena V, Agrawal BK. Estimation of serum zinc and alkaline phosphatase in malnourished children. Current Paed Research 2009; 12 (1): 10-12
Okolo SN, Okonji M, Ogonna C, Nwosu OK. And Ocheke MD. Serum zinc levels in malnourished pre- school Age attending the Jos University Teaching Hospital, Jos, Plateau state, Nigeria. Sahel Med J 2002; 5(4): 204-6
Mohammed MR, Mohammed A, George J.
Synergistic effect of zinc and Vitamin A on the biochemical indices of vitamin A nutrition in children. Am J Clin Nutr 2002; 75-92.
Nancy F. Krebs MD, Michael H. Normal childhood nutrition and its disorders: In Current Paediatric diagnosis and treatment, 16th ed. 2009; 277-307
Ugwuja El, Nwosu KO, Ugwu NC and Okoji M. Serum zinc and Copper levels in malnourished pre- school Age children in Jos, North Central Nig. Pakistan J of Nutr 2007; 6(4): 349-54
WHO child growth standards: length/heightfor-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: Methods and development. 2006:405
Araoye M.O. Sample size determination In: Research Methodology with Statistics for health and social sciences. Nathadex Publishers Saw- mill Ilorin2003; 115-21
Maziya-Dixon B, Akinyele IO, Oguntona EB, Nokoe S, Sanusi RA and Harris E. Nigeria Food Consumption and survey 2001-2003 Summary Report. International Institute of Tropical Agriculture, Ibadan, Nigeria; 2004.
Oyedeji GA. Socio-economic and Cultural Background of Hospitalized Children in Ilesha. Nig J Paed 1985; 12(4): 111-7
Ulasi TO, Ebenebe J. Nutritional disorders in children. In: Azubuike JC, Nkanginieme KEO Paediatrics and Child health in the tropical region 2nd ed, Owerri, University of Port Harcourt press 2007; 250-267
Kaneko JJ. Determination of minerals in serum and plasma. In: Clinical biochemistry of animals 4th ed. Academic press, New York; 2004:44-6.
Bruno B, Ian D, Lena D, Olivier F, Christian H. Conclusions of the joint WHO/ UNICEF/IAEA/ IZINNCG inter agency meeting on zinc status indicators. Food and Nutr Bull 2007; 28 (3):
-4.
Cartmel E, Natalal H, Francois I, Farara MH, Grahawt L. Nutritional and clinical status of children admitted to the malnutrition ward, Maputo central hospital: A comparison of data from 2001and 1983. J Trop paed 2005; 51:(2):
-5.
Agozie CU, Ngozi SI, Chika IN, Chinyeaka MU, Chinelo AN. Under five Protein Energy
Malnutrition admitted at the University of Nigeria Teaching Hospital, Enugu; A 10 year retrospective review. Accessed on line on 14th
S e p t e m b e r 2 0 1 6 a t http://www.nutrition.com/content/1/1/43.
Olwedo MA, Mworozi E, Bachou H, Orach GC. Factors associated with malnutrition among children in internally displaced person's camps, Northern Uganda. Afr Health Sci 2008 ;(8): 24452.
Emina JB, Kandala N, Inungu J. The effect of maternal education on child nutritional status in the Democratic Republic of the Congo, Nairobi, Kenya. J Public Health epidemiology2011;
(12) 576-92
Babatunde Omilola. Pattern and trends of child and maternal nutrition inequalities in Nigeria. 2010; International food policy research i n s t i t u t e a c c e s s e d o n l i n e a t
http://www.ifpri.org/sites/default/files/publicati ons/ifpridp00968.pdf on 18th September 2016
Kriti AP, Sanjivani DL, Naik JD, Rajderkar SS. Gender inequality and bio-social factors in nutritional status among under five children attending Anganwadis in an urban slum of a town in Western Maharashtra, India. J Res Med Sci 2013; 18(4): 341–45.
Madondo A, Macintyre UE, Ntuli B. Clinical and anthropometric profile of children. South Afr J of child health 2012; 6(4): 123-27.
Mary EP. Protein Energy Malnutrition, pathophysiology, clinical consequences and treatment. In: Walker AW, Christopher D, Watkim JB ed. Nutrition in Paediatrics. London. Blackwell Waterson. 2008; 171-84
Jelliffe DB. Protein-calorie malnutrition in tropical pre-school children. J Paed 1959; 54: 227-56
Werner S, Merzenich M, Rainer G, Shrimpton D. Effects of iron, zinc and vitamin A status of anaemic pre-school children in Indonesia. Public health nutrition, accessed on line on 18th
S e p t 2 0 1 6 a t
http://archives.unu.edu/unupress/food/v184e/c h1.htm.
Farhan J, Aneela A, Saifullah S, Mohammed A, Nadeem H, Bushra A. Comparison of serum zinc levels between healthy and malnourished children. A.P.M.C 2009; 3 (2): 139-42.
Anderson VP, Jack S, Monchy D, Hem N, Hok P, Balley KB et al. Co- existing micronutrients deficiencies among stunted Cambodian infants and toddlers. Asia Pac J Clin Nutr 2008; 17(1):
-9.
Jale E, Ayten MD, Ayhan O, Cardar MD. Hair zinc levels in healthy and malnourished children. Am J Clin Nutr 1978; 31:1172-4.
Mushi S. Mumbhi F. and Kitundal J.A. Zinc supplementation in children recovering from severe Protein Energy Malnutrition admitted at
M u h i m b i l i N a t i o n a l H o s p i t a l ,
DaresalamTanzania. Am J Clin Nutr 2008; 71:256-59.
Muzamil S. Stunting and micronutrients deficiencies in malnourished children. J Pak Med Assoc 2010; 60(7): 543-47
Diagnosis of zinc deficiency step by step, BMJ publishing group limited 2011, available at htp;/eso.cdn.bmj.com, accessed on 14th September 2016.
Solomon NW. Assesment of copper and zinc nutrition in man. Am J of Clin Nutr 1979; 32:856-71
Ivan SF, Jullio CD, Helio V, Alceu A, and Alexander A. Zinc serum levels and their association with vitamin A deficiency in preschool children. Jornal de paediastria 2007; 83:6:512-17.
Bemnet A, Beyene M, Bereket F, Ketema T, Desalegn W, Gizachew Y et al. Micronutrient levels and nutritional status of school children in North-west Ethiopia. Nutr J 2012; 11:108. Accessed on online www:nutrition. com on 14th September 2016.
Ugwuja El, Nwosu KO, Ugwu NC and Okoji M. Serum Zinc and Copper levels in malnourished pre- school Age children in Jos, North Central Nig. Pakistan J of Nutr 2007; 6(4): 349-54
Edward B, Edison M and Addy K. Serum zinc status of children with persistent diarrhea admitted to the diarrheoa management unit of Mulago Hospital, Uganda. Afr Health Sci 2003;3 (2): 54-60.
Deghanii SM, Katibeh P, Haghighat M, Moravel
H, Assad S. Prevalence of zinc deficiency in 318 years old children in Shiraz- Iran. Iran Red Crescent Med J 2011; 13 (1): 4-8
Abeer V, Nazir AM, Assad H, Riffat NA.
Evaluation of zinc status of preschool children as assessed by hair zinc levels in Punjab Province. Pakistan Armed Forces Medical Journal accessed online at http://www.pafmj.org On 14th September 2016.
Smit ZM, Preterius PJ. Serum zinc levels and urinary zinc excretions in South African Bantu kwashiorkor patients. J Trop Pediatr Environ Child health 1964; 9 (3): 105-12
Sanstead HH, Shukry AS, Prasad MK, Gabr A, Dabry WJ. Kwashiorkor in Egypt, Clinical and biochemical studies with special references to plasma zinc and serum lactic dehydrogenase.
Am J Clin Nutr 1965; 17 (5): 15:103-9.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Research Journal of Health Sciences

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Research Journal of Health Sciences journal is a peer reviewed, Open Access journal. The Journal subscribed to terms and conditions of Open Access publication. Articles are distributed under the terms of Creative Commons License (CC BY-NC-ND 4.0). (http://creativecommons.org/licences/by-nc-nd/4.0). All articles are made freely accessible for everyone to read, download, copy and distribute as long as appropriate credit is given and the new creations are licensed under the identical terms.

