Maternal death and near miss measurement: a case for implementation in developing countries in the sustainable development agenda, a review article.
Abstract
“Ending preventable maternal mortality (EPMM) remains an unfinished agenda and one of the world's most critical challenges. Maternal health, well-being and survival must remain a central goal and investment priority in the sustainable development goal agenda”. This statement from the World Health Organization (WHO) document Ending Preventable Maternal Death is most appropriate especially for developing nations.
Using 2010 as baseline, the current global maternal health targets are achievement of average maternal mortality ratio (MMR) of 70/100,000 live births. Nations whose MMR are more than 420/100,000 live births (the group where Nigeria belong) should have MMR not higher than 140 by 2030.
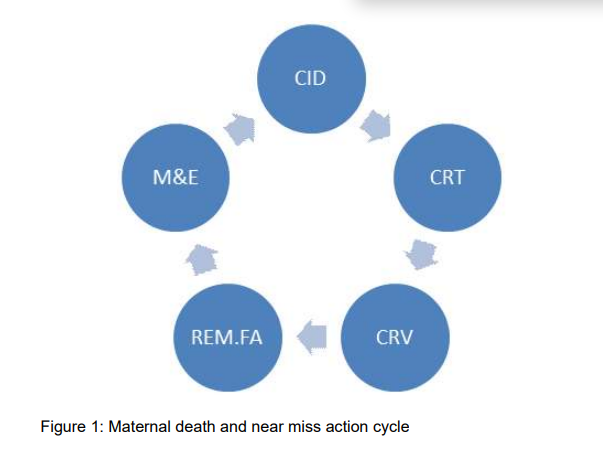
There was recognition of the need for improved measurement and data quality in other to track the progress or lack of it as we approach 2030. Maternal health services need to be accountable more than ever before. Maternal death and near miss measurement is one way to achieve this. In this paper a three levels of maternal death and near miss audit, surveillance and review is recommended for Nigeria and other developing nations. Both measurements can be done together.
Maternal death measurement also called maternal death review (MDR), audit or surveillance answers pertinent questions about the death of pregnant women, how many died? Where did they died? When did they died? Why did they died? Can these deaths be prevented? When MDR is followed by response (evidence base intervention) it becomes MDRS and thereby eliminates all preventable deaths. Every maternity service department and hospital, state and national government should audit the outcome of maternal health care being provided as a matter of accountability.
References
Lale Say, Doris Chou, Alison Gemmill, Özge Tunçalp, Ann-Beth Moller, Jane Daniels,
Metin Gülmezoglu A, Marleen Temmerman, Leontine Alkema. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014. 2: e323-33.
Yayla M: Maternal mortality in developing countries. J Perinat Med. 2003;31(5):386-91
WHO: Targets and Strategies for Ending Preventable Maternal Mortality EPMM. Human reproduction programme. hrp. research for impact. 2015.
World Health Organization. International classification of diseases (ICD) 10. Geneva,
W H O . 1 9 9 4 . A v a i l a b l e
fromh.ttp://www.who.int/classification/icd/en
/.
Federal Democratic Republic of Ethiopia Ministry of Health. Addis Ababa, Ethiopia. Maternal Death Surveillance and Response (MDSR) Technical Guideline. August, 2012.
John R. Wilmoth, Nobuko Mizoguchi, Mikkel
Z. Oestergaard, Lale Say, Colin D. Mathers, Sarah Zureick-Brown, Mie Inoue, and Doris Chou A New Method for Deriving Global Estimates of Maternal Mortality. Stat Politics Policy. 2012; 3(2): 2151-7509.1038.
Robert Pattinson , Lale Say, João Paulo Souza, Nynke van den Broek, Cleone Rooney & on behalf of the WHO Working Group on Maternal Mortality and Morbidity
Classifications WHO maternal death and nearmiss classifications. Bulletin of the World Health Organization 2009;87:734-734. doi: 10.2471/BLT.09.071001
Mantel GD, Buchmann E, Rees H, Pattinson RC. Severe acute maternal morbidity: A pilot study of a definition for a near-miss. Br J Obstet Gynaecol 1998; 105: 985-990.
Robert C Pattinson, Lale Say, JD Makin, Maria Helena Bastos . Critical incident audit and feedback to improve perinatal and maternal mortality and morbidity. Editorial Group: Cochrane Pregnancy and Childbirth Group Published Online: 19 OCT 2005. Assessed as u p - t o - d a t e : 11 J A N 2 0 11 D O I :
1002/14651858.CD002961.pub2
Julia Hussein and Friday Okonofua. Time for Action: Audit, Accountability and Confidential Enquiries into Maternal Deaths in Nigeria. Afr J Reprod Health 2012; 16[1]:9-145.
Althabe F, Bergel E, Cafferata ML, Gibbons L, Ciapponi A, Alemán A, Colantonio L, Palacios AR. Strategies for improving the quality of health care in maternal and child health in low- and middle-income countries: an overview of systematic reviews. Paediatr Perinat Epidemiol.2008; 22(Suppl 1):42-60.
Russell, Lesley. An Asclepiad family The Chamberlens and DeLaunes, 1569- 1792: Five generations of surgeons, physicians, accoucheurs and apothecaries. Journal of
Medical Biography. Sage Publications. Prepublished Online 26 June 2014.
Gary Cunningham. Williams Obstetrics, 14th edition. Appleton-Century-Crofts, New York, NY, 1971, pages 1116-8.
John William Ballantyne. The making of antenatal life:Teratology and the clinic. Wellcome History winter 2009. 42(2). 1-24.
Ulf Hogberg and Showall(1986) Secular trends in maternal mortality in Sweden from 17501980. Bulletine of the world health organization who. 64(1):79-84. Vincent De Brouwere, Vincent De Brouwere, Rene
Tonglet, Wim Van Lerberghe (1998).
Strategies for reducing maternal mortality in developing countries: What can we learn from the history of industrialized west. Tropical medicine and international health.3(10): 771782.
Editoria : Maternal mortality: An historical audit .Journal of the Royal College of General Practitioners, 1984, 34 585-588.
World Health Organization. Beyond the numbers: reviewing maternal deaths and complications to make pregnancy safer. Geneva. 2004.
Centre for Maternal and Child Enquiries (CMACE). Saving Mothers' Lives: reviewing maternal deaths to make motherhood safer: 2006–08. The Eighth Report on Confidential Enquiries into Maternal Deaths in the United Kingdom. BJOG 2011;118(Suppl. 1):1–203.
Wikipedia. Confidential Enquiry into Maternal Deaths in the UK. The free encyclopedia. last modified 24th November 2012.
WHO/UNICEF/UNFPA and The World Bank. Trends in Maternal Mortality: 1990-2010: Estimates developed by WHO,UNICEF, UNFPA and The World Basnk. Geneva, World Health Organization, 2012.
World Health Organization (WHO), UNICEF, UNFPA, and The World Bank, Trends in Maternal Mortality 1990–2008: Estimates Developed by WHO, UNICEF, UNFPA and The World Bank. Geneva: WHO, 2010.
A v a i l a b l e a t
www.who.int/reproductivehealth/publications /monitor-ing/9789241500265/en/index.html.
United Nations General Assembly, United Nations Sustainable Development Goals SDG.New York. United Nation Publication 2015: A/69/85;1-35.
World Health Organization. Trends in maternal mortality: 1990 to 2013. Estimates by WHO, UNICEF, UNFPA, The World Bank and the United Nations Population Division. Geneva:
W H O ; 2 0 1 4 . A v a i l a b l e f r o m
http://www.who.int/reproductivehealth/public ations/monitoring/maternal-mortality-
/en/ [cited 2014 Jul 18].
World Health Organization (WHO), Maternal Death Surveillance and Response. Technical Guidance. Information for action to prevent maternal death. WHO 2013.
National Population Commission (NPC) {Nigeria}and ICF Macro. 2009 Nigeria
Demographic and Health Survey 2008 . Abuja, Nigeria. National population commission and ICF macro.
National Population Commission (NPC)
{Nigeria}and ICF International 2014. Nigeria Demographic and Health Survey 2013. Abuja, Nigeria. And Rockville, Maryland, USA: NPC and ICF International.
Adeleke NA Olowookere SA. Pattern of Maternal Mortality in a General Hospital Osogbo South Western Nigeria. Nig. Medical practitioner 2011. 59 (5-6): 68-75
Amatare Dinyain, G Olutoyin Omoniyi-Esan, Olaejirinde O Olaofe, Donatus Sabageh, Akinwumi O Komolafe, and Olusegun S Ojo.
Autopsy-certified maternal mortality at Ile-Ife, Nigeria.Int J Womens Health.; 2014. 6: 41–46.
Galadanci H, Künzel W, Zinser R, Shittu O, Adams S, Gruhl M. Experiences of 6 years quality assurance in obstetrics in Nigeria - a critical review of results and obstacles. J Perinat Med. 2015. doi: 10.1515/jpm-2014-
[Epub ahead of print]
Betrán AP, Wojdyla D, Posner SF, Gülmezoglu AM (2005).National estimates for maternal mortality: an analysis based on the WHO systematic review of maternal mortality and morbidity. BMC Public Health. 2005 12;5:131
WHO, UNICEF, UNFPA, The World Bank, and United Nations Population Division Maternal Mortality Estimation Inter-Agency Group. Maternal mortality in 1990-2013 World population prospects: the 2012 revision. New York, Population Division, Department of Economic and Social Affairs, United Nations Secretariat, 2013.
Stanton C, Abderrahim N, Hill K. An assessment of DHS maternal mortality indicators. Stud Fam Plann 2000; 31: 111-23.
Gakidou E, Hogan M, Lopez AD. Adult mortality: time for a reappraisal. Int J Epidemiol. 2004; 33: 710-7.
Adinma B-DJI, Adinma. ED A critic of maternal mortality reduction efforts in Nigeria. Trop. Jour. 2011. 28(1): 45-48.
Samuel Mills (HDNHE, World Bank).
Maternal Death Audit as a Tool to reducing Maternal Mortality. HNPNotes. 2011.
Achem FF, Agboghoroma CC. Setting up facility-based maternal death reviews in Nigeria. BJOG 2014; 121 (Suppl. 4): 75–80.
Eugene J Kongnyuy and Nynke van den Broek. The difficulties of conducting maternal death reviews in Malawi. BMC Pregnancy and Childbirth 2008: 8(42) 1471-2393.
Cook R.The role of confidential enquiries in the reduction of maternal mortality and alternatives to this approach. Int J Gynaecol Obstet. 1989 ;30(1):41-5.
Hussein J. Improving the use of confidential enquiries into maternal deaths in developing countries. Bull World Health Organ. 2007; 85(1): 68-69.
Thorsen VC, Johanne Sundby, Tarek Meguid and Address Malata. Easier said than done!: methodological challenges with conducting maternal death review research in Malawi. BMC Medical Research Methodology
,14:29.
Graham WJ, Ahmed S, Stanton C, Abou-Zahr C, Campbell OM. Measuring maternal mortality: an overview of opportunities and options for developing countries. BMC Med. 2008 May 26;6:12.
Graham W, Wagaarachchi P, Penney G,
McCaw-Binns A, Antwi KY, Hall MH. Criteria for clinical audit of the quality of hospitalbased obstetric care in developing countries. Bull World Health Organ. 2000;78(5):614-20.
Hussein J, D'Ambruoso L, Armar-Klemesu M,
Achadi E, Arhinful D, Izati Y, Ansong-Tornui J.
Confidential inquiries into maternal deaths: modifications and adaptations in Ghana and Indonesia. Int J Gynaecol Obstet. 2009 ;106(1):80-4.
Samuel Hailu Fikre Enqueselassie Yemane Berhane. Health facility-based maternal death audit in Tigray, Ethiopia. Ethiop. J. Health Dev: 2009. 23(2): 115-119.
Oladapo OT, Adetoro OO, Ekele BA, Chama C, Etuk SJ, Aboyeji AP, et al. Nigeria Nearmiss and Maternal Death Surveillance Network. When getting there is not enough: a nationwide cross-sectional study of 998 maternal deaths and 1451 near-misses in public tertiary hospitals in a low-income country. BJOG 2015; 10.1111/1471-0528.13450
Ina May Gaskin, CPM, MA. Maternal Death in the United States: A Problem Solved or a Problem Ignored? J Perinat Educ. 2008; 17(2): 9–13.
Lawal Oyeneyin. Institutionalizing a Maternal Death Review System Case study of Ondo State Abiuye (Safe motherhood) Programme. Trop. J. Obstet. & Gynaecol. 30 (suppl. 1), November 2013: S38.
www.sogon.org.ng Development diaries (2015) Nigeria: MacArthur Maternal Health Portfolio Accountability Baseline Report. Posted on May 1, 2015.
Maternal Mortality in New Jersey, 1999-2001. New Jersey department of health and senior services. 2005.
Thaddeus S and Maine D. “Too far to walk: maternal mortality in context,” Social Science and Medicine. 1994. 38(8):1091–1110.
Barnes-Josiah D, Myntti C, Augustin A. The "three delays" as a framework for examining maternal mortality in Haiti. Soc Sci Med. 1998. 46(8):981-93.
Van Dillen J, Stekelenburg J, Schutte J, Walraven G, van Roosmalen J. The use of audit to identify maternal mortality in different settings: is it just a difference between the rich and the poor? Healthc Q. 2007 ;10(2):131-7.
Lewis G. The cultural environment behind successful maternal death and morbidity reviews. BJOG. 2014: 121 (Suppl. 4): 24–31
Maternal Death Survillance and Review MDSR Action Network's newsletter! March 2015 edition.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Research Journal of Health Sciences

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Research Journal of Health Sciences journal is a peer reviewed, Open Access journal. The Journal subscribed to terms and conditions of Open Access publication. Articles are distributed under the terms of Creative Commons License (CC BY-NC-ND 4.0). (http://creativecommons.org/licences/by-nc-nd/4.0). All articles are made freely accessible for everyone to read, download, copy and distribute as long as appropriate credit is given and the new creations are licensed under the identical terms.

