Atrial fibrillation: An analysis of etiology and management pattern in a tertiary hospital in Port-harcourt, southern Nigeria
Keywords:
Atrial fibrillation, thrombosis, CHADS2 Score, stroke risk, hypertensive heart disease, cadiomyopathyAbstract
Objective: Atrial fibrillation is the commonest chronic arrhythmia and the etiology is widely varied. The aim of this study was to determine the etiology, clinical characteristics and treatment offered to adult patients with atrial fibrillation managed in a referral hospital in Port Harcourt, southern Nigeria.
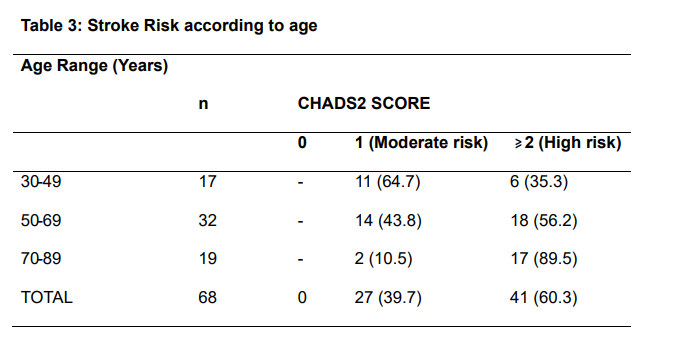
Methods: A retrospective study of all the patients referred to the cardiology unit or seen in the cardiac clinic with ECG evidence of atrial fibrillation over one year period July 2012 to June 2013 was carried out. Those with confirmed atrial fibrillation and had transthoracic echocardiographic evaluation were analyzed for the study. Clinical and demographic characteristics and treatment offered to the patients were obtained from their hospital notes. Stroke risk was retrospectively assessed using the CHADS2 score.
Results: Sixty-eight patients comprising twenty nine females and thirty nine males [ratio of 1;1.3] had complete data . Age range was 30-87 years and mean age was 59.81±14.22 years. Mean blood pressures were 126.03± 26.89 mmHg systolic and 67.22± 18.60 mmHg diastolic. Hypertensive heart disease was the diagnosis in forty patients [58.82%], dilated cardiomyopathy in thirteen [19.2%], rheumatic heart disease in ten [14.71%], thyrotoxicosis in three [4.41%], one each due to endomyocardial fibrosis [EMF] and Cor pulmonale. Ten patients (14.71%) had valvular atrial fibrillation (AF) while most [ 85.29%] had non-valvular AF. None of the patients had evidence of stroke risk evaluation in their notes and less than 10% received anticoagulation treatment despite all the patients having moderate to high risk of stroke from our own CHADS2 evaluation.
Conclusion: Hypertensive heart disease was the commonest cause of atrial fibrillation in patients seen Port Harcourt, Southern Nigeria, followed by dilated cardiomyopathy and rheumatic heart disease. Stroke risk evaluation was non-existent and adherence to guidelines in management of atrial fibrillation was suboptimal.
References
Benjamin EJ, Wolf PA, DAgostino RB,
Sibbershatz H, Kannel WB, and Levy D. Impact of Atrial Fibrillation on risk of death: The Framingham heart study. Circulation
;98(10):946-52.
Kirchhof P, Auricchio A, Bax J, Crijins A, Camm J, Diener HC, et al. Outcome parameters for trials in atrial fibrillation; executive summary. Recommendation from a concensus conference organized by the German Atrial Fibrillation
Competence Network (AFNET) and the European Heart Rhythm Association (EHRA).
Eur Heart J 2007;28:2803-2817.
Lip GY, Golding DJ, Nazir M, Beavas DG, Child DL, Fletcher RI. A survey of Atrial fibrillation in general practice: The West Birmingham Atrial Fibrillation Project. Br J Gen Practice 1997;47: 28.
Thomas Cooke, Antje Groth, Sabrins Mueller, Mathias Pfannkuche, Frank Verheyen, Roland
Linder, et al. Incidence and prevalence of Atrial Fibrillation: An analysis based on 8.3million patients. Europace 2013;15(4): 486-493.
Mbakwem AC, Ajuluchukwu JNA, Oke DA. Clinical, Electrocardiographic and
Echocardiographic features of Atrial fibrillation in Nigerians: An Analysis of 39 patients seen at the University of Lagos Teaching Hospital.
Nigerian Quarterly J Hosp Med 2002;12(1-4)2933.
Massane Mbaye, Soulemane Pessinaa, Malick Bodian, Bamba N. Moutamadon, Faton Mbaye, Adama Kane et al. Atrial fibrillation, frequency, etiologic factors, evolution and treatment in a cardiology department in Dakar, Senegal. Pan Afr Med J 2010;6:16.
Marie Ntep-Gweth, Marc Zimmermann,
Alexandre Meiltz, Samuel Kingue, Piere Ndobo, Philip Urban, ? et al. Atrial Fibrillation in Africa:
Clinical Characteristics, Prognosis, and adherence to guidelinesin Cameroon. Europace 2010; 12: 482-487.
Friberg L, Hamman N, Ringh M, Petterson H, Rosenqvist M. Stroke prophylaxis in Atrial fibrillation: who gets it and who does not? Eur Heart J 2006;27:1954-64.
Lip GY, Edwards SJ. Stroke prevention with aspirin, warfarin and ximelagatran in patients with non-valvular atrial fibrillation: a systematic review and meta-analysis. Thromb Res 2006; 118:321–33.
Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have non valvular atrial fibrillation.
Ann Intern Med 2007; 146: 857–67.
Mant J, Hobbs FD, Fletcher K, Roalfe A, Fitzmaurice D, Lip GY AND Murray E.. Warfarin versus aspirin for stroke prevention in an elderly community population with atrial fibrillation (the Birmingham Atrial Fibrillation Treatment of the Aged Study, BAFTA): a randomised controlled trial. Lancet 2007;370: 493–503.
Bhagat K, Tisocki K. Prescribing patterns for the use of antithrombotics in the management of atrial fibrillation in Zimbabwe. Cent Afr J Med 1999;45:287–90.
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Research Journal of Health Sciences

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Research Journal of Health Sciences journal is a peer reviewed, Open Access journal. The Journal subscribed to terms and conditions of Open Access publication. Articles are distributed under the terms of Creative Commons License (CC BY-NC-ND 4.0). (http://creativecommons.org/licences/by-nc-nd/4.0). All articles are made freely accessible for everyone to read, download, copy and distribute as long as appropriate credit is given and the new creations are licensed under the identical terms.

